SVT (supraventricular tachycardia) is a common kind of arrhythmia (abnormal heart rhythm). With SVT, your heartbeat is too fast and starts in your heart’s upper chambers. You may or may not have symptoms like chest pain or dizziness. There are some things you can do on your own, but you may need medicine or surgery to help with symptoms.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
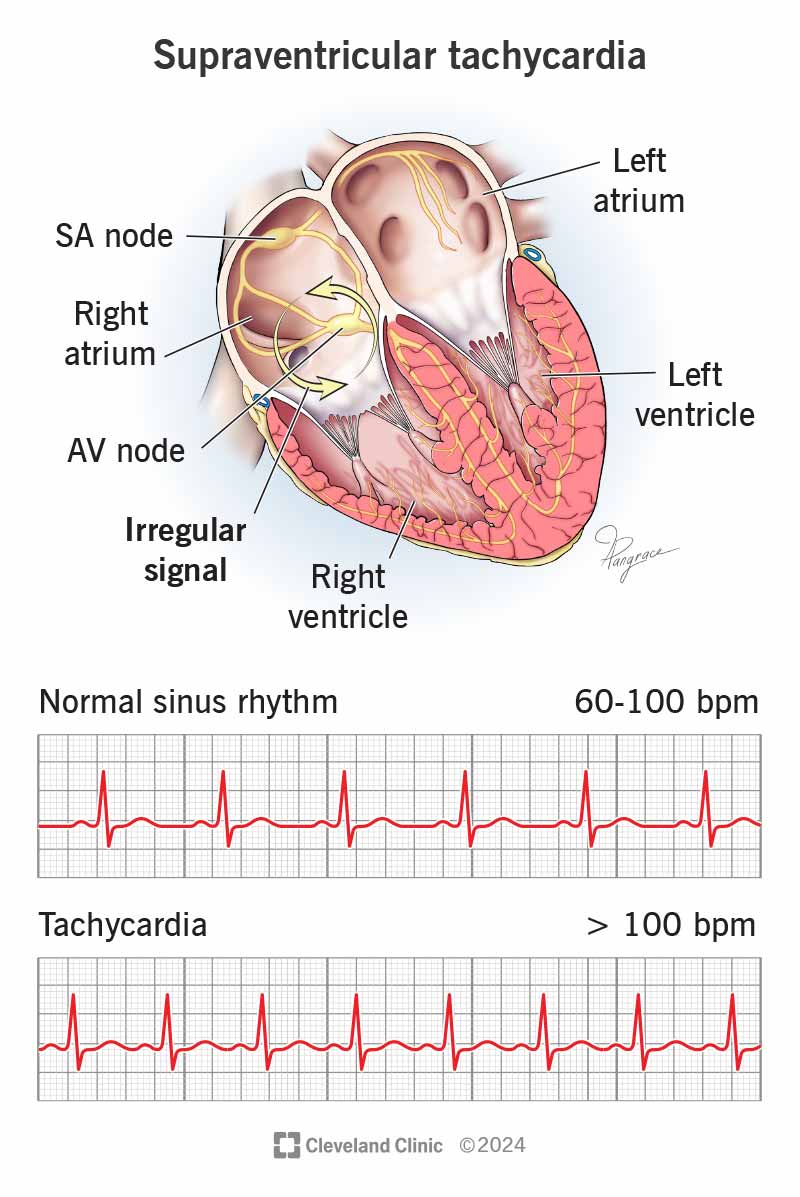
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/supraventricular-tachycardia)
Supraventricular tachycardia (SVT) is a fast heart rate that starts in your upper heart chambers. When your heart is beating too fast at rest, it makes it hard to send enough blood to your body. Episodes can go on for seconds to hours.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
When your heart beats too quickly, there’s not enough time for your heart chambers to fill with blood before they contract.
If you have symptoms, you may think something doesn’t feel right in your chest. Although it may be difficult, noting the details of what you’re experiencing can help a healthcare provider make a diagnosis.
Different kinds of SVT include:
You might not have any symptoms with SVT. But whether you realize it or not, your heart’s beating more than 100 times per minute while at rest.
Other supraventricular tachycardia symptoms may include:
Symptoms may range from mild to severe.
A problem with your heart’s electrical signals or circuitry causes SVT. Some people may not be aware of what brings their symptoms on. Others have a clear “trigger” that starts their SVT. Supraventricular tachycardia causes that can bring about symptoms include:
Advertisement
Children and adults can get supraventricular tachycardia. Risk factors for SVT include:
A serious case of SVT may lead to:
SVT isn’t life-threatening in most cases, but it can be for people with other heart issues.
During a physical exam, your healthcare provider will ask about your medical history and the symptoms you’ve been having.
They’ll most likely do an electrocardiogram (EKG or ECG). If your provider needs to study your heart for a longer amount of time, they may ask you to wear a heart monitor that records the electrical activity in your heart.
You may not need SVT treatment. Some people may feel better after resting more, drinking less coffee or alcohol-containing drinks, or after quitting smoking. If those don’t help, you have lots of other options.
Try one of these first:
Several medicines can slow down your heart rate:
If your healthcare provider prescribes medicines for you, be sure to follow the instructions for taking them. Also, keep going to your follow-up appointments.
Your provider can use these methods for supraventricular tachycardia treatment:
Any medicine may have side effects. Although a catheter ablation has a low risk of major complications, it may cause:
Vagal maneuvers and at-home treatments can bring relief right away — if they work. Medicines and procedures are more reliable but take longer to work. If you’re having an SVT episode, it’s worth trying at-home treatments. For the long term, you may need medicines or procedures.
Advertisement
The outlook is good for most people with SVT. But if you have a structural issue with your heart, your prognosis (outlook) may not be as good. It depends on the severity of the problem.
Yes. You can manage very infrequent episodes with medications. With successful treatments like catheter ablation, you can do many of the typical things you want to. Ablation can cure certain forms of SVT.
If SVT is from causes you can change, you can:
You should also keep taking the medicine your healthcare provider prescribed for you.
Changes you make in your daily routines can help with SVT (supraventricular tachycardia). You can:
You should also continue taking your prescription medications.
You should see your provider if you have symptoms of SVT (supraventricular tachycardia), including:
Advertisement
Call 911 or your local emergency services number if you:
Questions to ask your provider may include:
It’s frustrating and concerning to feel like something isn’t right with your heart. But once you have an SVT (supraventricular tachycardia) diagnosis, you’re on your way to a solution. Ask your healthcare provider which treatment is best for you. There may be simple things you can do to help with symptoms. Be sure to keep taking medicine prescribed to you and keep up with follow-up appointments.
Advertisement

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
When your heart rhythm is out of sync, the experts at Cleveland Clinic can find out why. We offer personalized care for all types of arrhythmias.
