Heart block is a problem with your heartbeat signal moving from the upper to lower part of your heart. The signal can only get through sometimes, or not at all. This makes your heart beat slowly or skip beats. People with second-degree or third-degree heart block may experience fainting, tiredness and shortness of breath.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
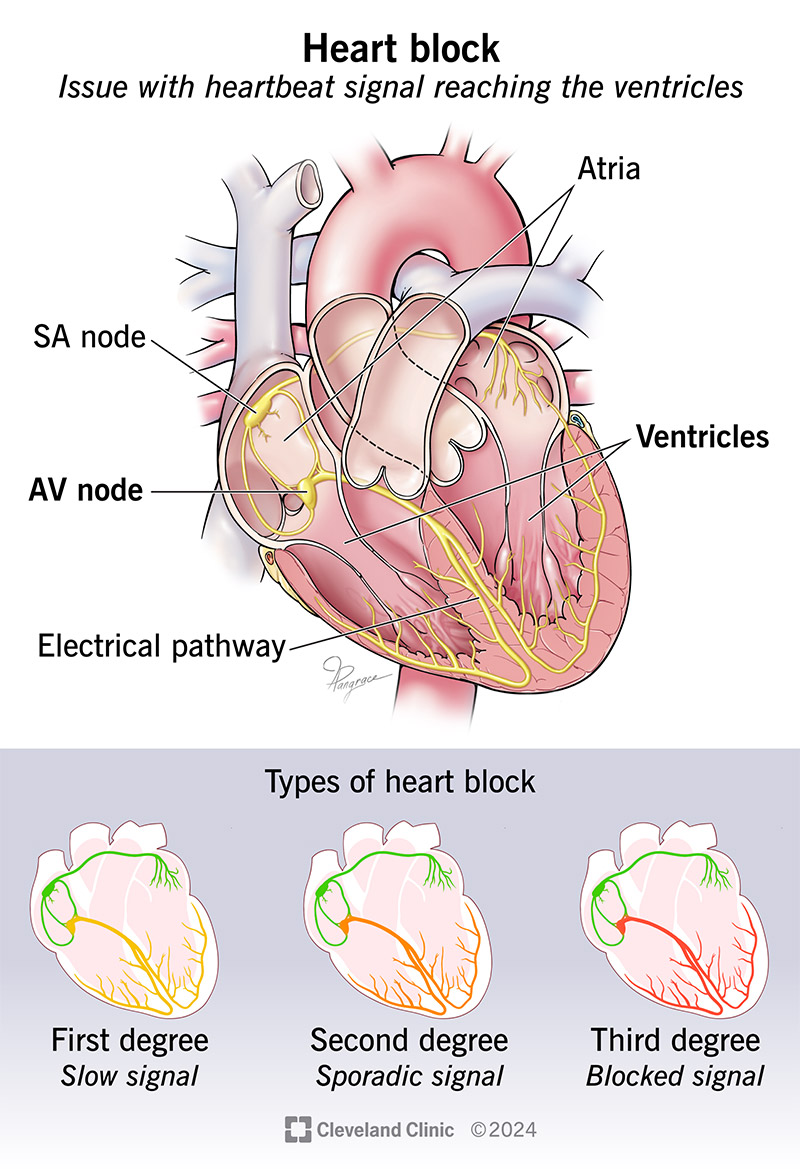
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/17056-heart-block)
Heart block is an issue with a heartbeat signal traveling from the top chambers of your heart to the bottom chambers of your heart. Normally, electrical signals (impulses) travel from your heart’s upper chambers (atria) to your lower chambers (ventricles). The signal moves through your AV node, a cluster of cells that link the electrical activity from your top to bottom chambers. If you have heart block, the signal only makes it to your ventricles some of the time, if at all.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
The result is a heart that may not work well. Your heart may beat slowly or skip beats. In severe cases, heart block can affect your heart’s ability to pump blood, causing low blood flow to your entire body.
People are more likely to acquire heart block later in life than to have it at birth.
Other names for heart block are atrioventricular (AV) block or a conduction disorder.
Heart blocks can range from mild to severe, depending on whether the electrical signal can get through, and how often. Heart block types are:
First-degree heart block: The electrical impulse still reaches your ventricles, but moves more slowly than normal through the AV node. This is the most mild type of heart block.
Second-degree (incomplete) heart block: With this type, your heart’s impulses only get to the lower chambers some of the time. The types of second-degree heart block are:
Advertisement
Third-degree heart block: This is a complete blockage of the electrical signal from your atria to your ventricles. Third-degree block negatively affects your heart’s ability to pump blood out to your body. This form of heart block is serious and usually requires a pacemaker for treatment.
Symptoms of heart block vary depending on the severity of the block and how it affects the heart pump.
Heart block symptoms may include:
People with first-degree heart block may not have any symptoms. A provider may find first-degree heart block during a routine electrocardiogram (EKG).
Symptoms of third-degree heart block are more intense due to the slow heart rate. If you have severe symptoms, get medical attention right away.
Causes of heart block include:
You may be at an increased risk of a heart block if:
The complications can be life-threatening and include:
To diagnose heart block, your healthcare provider will:
Advertisement
Your cardiologist may refer you to an electrophysiologist, an expert in the electrical activity of your heart.
Tests you might have include:
Heart block treatment varies from person to person. A provider may admit you to the hospital to monitor your heart. To manage your condition, your cardiologist will consider:
Sometimes, making changes to medicines or treatment for heart disease stops heart block. Other people may need a temporary or permanent pacemaker that sends electrical pulses to their hearts.
If you need a pacemaker, your provider will talk to you about the details, the type that’s best for you, and what to expect before, during and after you get your pacemaker.
Advertisement
If you receive a temporary or permanent pacemaker, you may have side effects like:
After receiving a pacemaker, you may need to stay overnight in the hospital. You should be able to get back to your regular activities a few days to weeks after surgery. Ask your provider for specific restrictions after the procedure.
If you have first-degree heart block, ask your cardiologist or electrophysiologist what — if any — changes you need to make to your lifestyle or medications. This type of heart block doesn’t usually get in the way of your normal activities.
In general, a pacemaker won’t seriously restrict your ability to take part in sports and leisure activities. It’s important to follow your provider’s instructions for pacemaker monitoring so they can ensure your device is working correctly.
The cause of your heart block determines how long it lasts. If you replace a medication that causes heart block, that can resolve the issue. But heart block from another cause will likely be a lifelong condition.
Heart blocks can be serious. Without treatment, severe heart block can cause sudden cardiac arrest. But most commonly, untreated heart block can cause lightheadedness or fainting spells.
Advertisement
With treatment, your outlook depends on your age and what other conditions you have.
You may be able to prevent some causes of heart block, like heart disease.
Steps you can take to keep your heart and body as healthy as possible include:
If you have a pacemaker:
If you have a pacemaker, your cardiologist will want to check it periodically to make sure that it continues to work well. They can monitor you remotely, but you’ll need annual in-person appointments when your provider evaluates and adjusts your pacemaker.
Call your healthcare provider if you experience:
You need immediate medical care if you have a heart attack or cardiac arrest. Let your family and co-workers know about your risk of these (and the symptoms) so they can call 911 or your local emergency number.
Questions to ask your healthcare provider may include:
It can be unnerving to have chest pain or have trouble catching your breath. But getting a heart block diagnosis can explain why you’re experiencing those symptoms. The good news is that people who need treatment can have success with medicines or pacemakers that keep their hearts in a normal rhythm. Be sure to ask your provider about anything that isn’t clear when discussing your treatment plan.
Learn more about the Health Library and our editorial process.
Cleveland Clinic's health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability, and up-to-date clinical standards.
Cleveland Clinic's health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability, and up-to-date clinical standards.
When your heart rhythm is out of sync, the experts at Cleveland Clinic can find out why. We offer personalized care for all types of arrhythmias.
