Obstructive sleep apnea (OSA) is when you stop breathing during sleep because of a blockage in your windpipe. You may wake up frequently, which can lead to daytime exhaustion and other frustrating symptoms. Untreated OSA increases your risk of life-threatening complications. A healthcare provider might recommend lifestyle changes or using a CPAP machine.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
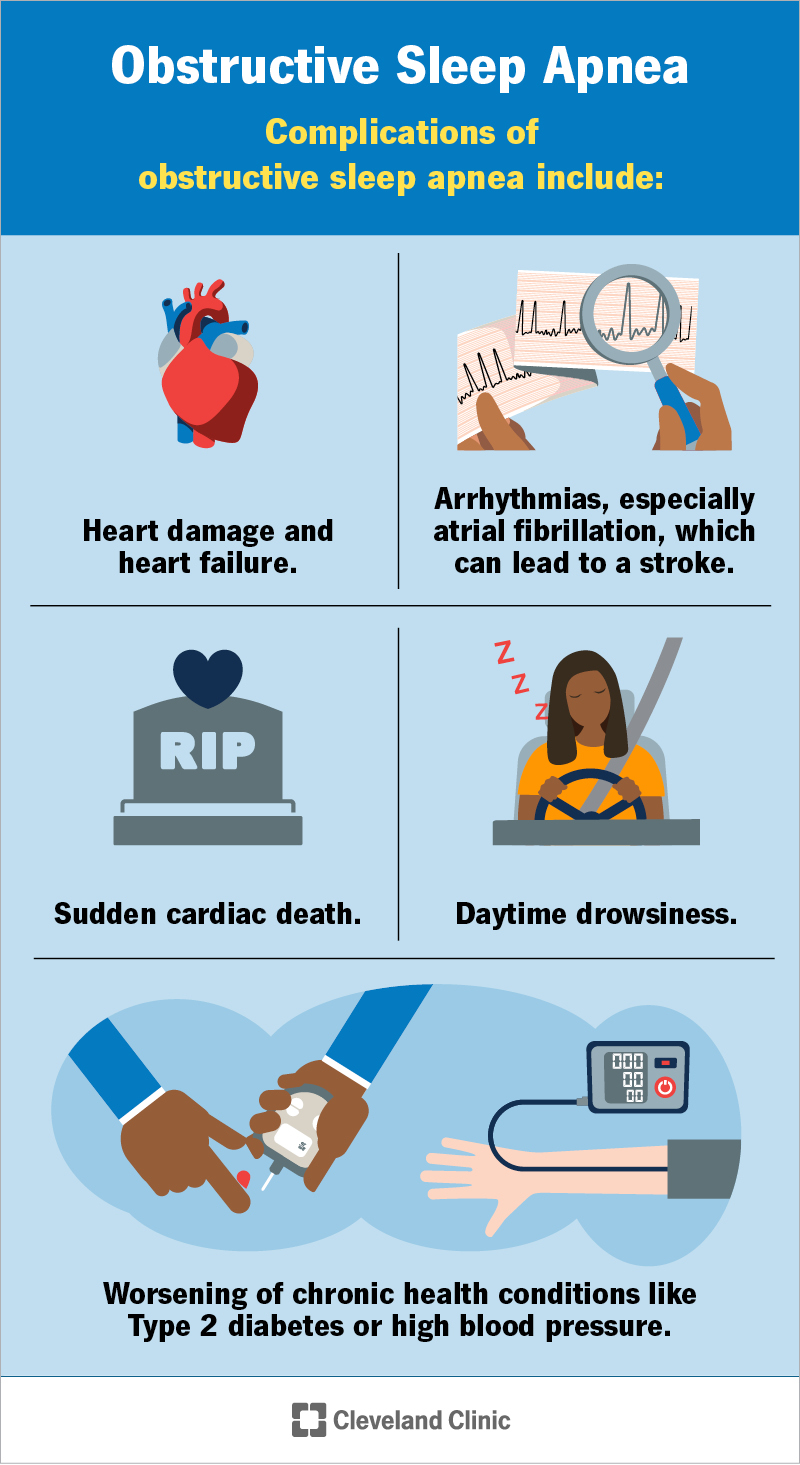
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/24443-obstructive-sleep-apnea)
Obstructive sleep apnea (OSA) is a condition where a blockage or narrowing in your airway keeps air from moving through your windpipe when you’re asleep.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
The blockage and lack of airflow can cause your blood oxygen levels to drop. This triggers a survival reflex in your brain that wakes you up just enough to breathe again. While that reflex is key in keeping you breathing, it also disrupts your sleep.
If you have frequent wakeups at night, you won’t feel rested in the morning. That can lead to a wide range of symptoms, many of which can affect your daytime functioning. Over time, these symptoms can lead to dangerous and sometimes life-threatening complications.
A healthcare provider can help you manage symptoms of OSA.
OSA affects up to 1 billion people around the world who are between the ages of 30 and 69.
Symptoms of obstructive sleep apnea that you or a sleeping partner will notice at night include:
Daytime symptoms may include:
You might notice the following characteristics in a sleeping partner who has OSA:
Advertisement
A blockage in your upper airway causes obstructive sleep apnea. Your muscles relax when you sleep, even the ones that allow air to flow into your lungs. But there should still be enough room for air to get into your body. With sleep apnea, relaxed muscles and tissues block the airway. This prevents airflow, which causes you to stop breathing.
OSA can happen to anyone at any age or any body size. It’s more common if you have any of the following:
OSA is more common as you age but it can also affect children.
Obstructive sleep apnea can lead to dangerous and sometimes life-threatening complications that may include:
A healthcare provider will diagnose OSA after taking your medical history, performing a physical exam and recommending tests. During the exam, your provider will examine your mouth, neck and throat. They’ll also ask you about what symptoms you experience at night and during the daytime.
Two tests can help diagnose OSA, including:
If you suspect you or a loved one has OSA, you might be able to help a healthcare provider diagnose it. You can take video and audio recordings of the person sleeping with their permission. This key evidence may help speed up the diagnostic process.
Treatment for OSA may include:
Common types of surgeries to open your airway and treat OSA include:
Advertisement
Untreated OSA may reduce your life expectancy and increase your risk of dangerous complications. But OSA is a treatable condition. A healthcare provider is the best person to talk to about what you can expect, as this answer is very unique to you.
The outlook for OSA depends on many factors like the severity and whether you have other underlying conditions, too. However, you can expect a positive outcome if you stick to your treatment plan after you and your healthcare provider find one that works best for you.
You can’t prevent all cases of OSA. But you can take steps to reduce your risk and improve your overall sleep by:
Advertisement
Visit a healthcare provider if you suspect you or a loved one have symptoms of sleep apnea. It may help to record your breathing at night so your provider can learn more about what’s going on.
If you have OSA, stay regular with your follow-up appointments. Your provider will want to make sure your treatment is working effectively. Be honest with them if you’re having trouble wearing a PAP mask at night or changing your sleeping habits. They may have recommendations to make things easier.
If you have trouble breathing when you wake up or have symptoms of potentially life-threatening complications like a heart attack (chest pain, heartburn, cold sweats) or stroke (sudden weakness or numbness on one side, confusion, dizziness), contact your local emergency services number right away.
If you have OSA, you can ask your provider:
Sleeping through the night with obstructive sleep apnea (OSA) can be a challenge. But achieving restful sleep doesn’t have to be a dream. OSA is a manageable condition. Many people see symptom relief by following their provider’s treatment plan. It may be difficult at first to change up your nighttime routine, but it should feel easier as you get used to it. Let your provider know if you run into any pitfalls, like PAP mask fitting or position changes while sleeping. They may have recommendations to help you stay comfortable.
Advertisement

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Obstructive sleep apnea can keep you from the getting the good night’s rest you need. Cleveland Clinic’s experts can create a treatment plan that helps.
