Overview
Cancers of the Reproductive System
What is gynecologic cancer?
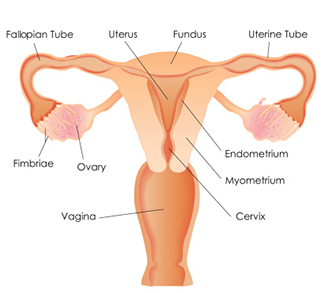
Gynecologic cancers affect a woman’s reproductive organs, including cervix, uterus, ovaries, fallopian tubes, vagina and vulva. The American Cancer Society estimates each year, approximately 106,000 women are diagnosed with a cancer of the reproductive organ including ovarian cancer, uterine cancer, cervical cancer and vulvar cancer.
What is a gynecologic oncologist?
A gynecologic oncologist is a physician first trained in obstetrics and gynecology who has an additional three to four years of training in gynecologic cancers including advanced surgery techniques and chemotherapy administration. These gynecologic oncology specialists use these skills to treat cancers of the female reproductive system.
Cleveland Clinic gynecologic oncologists are among approximately 1,000 physicians in the United States who are board certified in gynecologic oncology, as well as obstetrics and gynecology by the American Board of Obstetrics and Gynecology.
A Team Approach
Cleveland Clinic’s team approach of involving multiple specialists can be the most important factor in cancer treatment. Our oncologists work closely with gynecologic pathologists, radiation oncologists, radiologists, nurse practitioners and physician assistants. Together, they provide a careful blend of accurate diagnosis, surgical skill, leading-edge radiation therapy, advanced chemotherapy and compassionate care.
We understand the fear and uncertainty a diagnosis of cancer can bring. Our specialized team includes nurse practitioners/physician assistants who are licensed independent providers that will work with your gynecologic oncologist to provide care and help coordinate your cancer treatment. Our team also includes nurse navigators, chemotherapy coordinators and social workers who will provide supportive care and patient education. Our multidisciplinary team is here to help you throughout this difficult time
What We Treat
Who is at risk for gynecologic cancer?
The following are risk factors for different kinds of gynecologic cancers. Each cancer has its own general risk factors, and may affect women in various ways. Every woman is different, so talk to your doctor or gynecology oncology specialist about any questions or concerns you may have.
Risk factors include:
- Post menopausal (over age 50)
- Endometrial hyperplasia – a condition where the cells of the endometrium are abnormal
- Cervical intraepithelial neoplasia (CIN), also known as cervical dysplasia
- Obesity
- Diabetes
- High blood sugar
- Other cancers (colon, rectal, breast)
- Early age of first menstruation
- Women who have never been pregnant
- Hormone-related issues
- Family history of breast or ovarian cancer
- Download our Guide to Gynecological Cancer
Gynecology Oncology is a discipline that focuses on the treatment of cancers of a gynecologic nature. To learn more about gynecology and oncology topics, including types of cancer, their treatments, and more, please review the resources available here.
Services
What gynecology oncology services are provided at Cleveland Clinic?
- Access to the latest techniques in the management of gynecologic cancers including the newest drug treatments and access to clinical trials through our membership in NRG Oncology, sponsored by the National Cancer Institute.
- Minimally invasive surgery (including robotic-assisted laparoscopy and single port laparoscopy) used in the management of some early gynecologic cancers, including lymph node dissections and other staging procedures.
- A gynecologic chemotherapy unit with private infusion rooms is located within the department for patient convenience and is staffed by specially trained oncology nurses with chemotherapy certification.
- Hyperthermic (or Heated) Intraoperative Peritoneal Chemotherapy (HIPEC), which is an alternative and innovative method of delivering chemotherapy, commonly used to treat cancers that have spread to the lining of the abdominal cavity.
- The Radiation Therapy Center provides the latest, most sophisticated radiation therapy techniques for treatment of gynecologic cancers including custom brachytherapy, interstitial radiation, external beam radiation therapy, intensity-modulated radiation therapy (IMRT), and intra-operative radiation therapy (IORT).
- Ultrasound with color flow Doppler imaging for identifying blood flow changes associated with early ovarian cancer.
- Colposcopy which is an office procedure where a specialized microscope (called a colposcope) is used to examine the cervix, vagina or vulva for pre-cancerous cells.
- The Loop Electrosurgical Excision Procedure (LEEP), which is an office procedure to safely and comfortably remove pre-cancerous cells from the cervix without having to undergo a procedure in an operating room under anesthesia.
Cervical Cancer Screening
Thanks to recent advances in understanding the cause of cervical cancer, screening for this disease has now become more accurate and therefore more preventable.
Cervical cancer is caused by the presence and persistence of the human papilloma virus (HPV), a very common sexually transmitted disease. The combined use of HPV testing and the traditional pap test, especially in women over the age of 30 is now the new standard. Additionally, the availability of the HPV vaccine will likely reduce the number of cervical cancer cases in the future.
Resources
Cervical cancer gynecology oncology resources
Overview: Cervical Cancer, HPV, HPV Vaccine, Cervical Dysplasia
Prevention: Cervical Cancer Screening Guidelines
Diagnosis: When a Pap Test is Abnormal
Treatment: LEEP
Ovarian cancer
Overview: Ovarian Cancer
Care & Treatment: Ovarian Epithelial Cancer / Ovarian Germ Cell Tumor
Genetic Aspects: Breast and Ovarian Cancer
There is no standard screening protocol for ovarian cancer unless the patient is a member of a high-risk family with a history of breast and/or ovarian cancer. Your physician can help you determine whether you need to be tested for ovarian cancer
Uterine Cancer
Overview: Uterine (Endometrial) Cancer
Vaginal Cancer
Overview: Vaginal Cancer
Our Doctors
Looking for a gynecologic oncologist?
Find a ProviderAppointments
To make an appointment with one of our specialists, please call 216.444.6601 (toll-free 800.223.2273 ext. 46601).
Virtual Second Opinions
If you cannot travel to Cleveland Clinic, help is available. You can connect with Cleveland Clinic specialists from any location in the world via a phone, tablet, or computer, eliminating the burden of travel time and other obstacles.
If you’re facing a significant medical condition or treatment such as surgery, this program provides virtual access to a Cleveland Clinic physician who will review the diagnosis and treatment plan. Following a comprehensive evaluation of medical records and labs, you’ll receive an educational second opinion from an expert in their medical condition covering diagnosis, treatment options or alternatives as well as recommendations regarding future therapeutic considerations. You’ll also have the unique opportunity to speak with the physician expert directly to address questions or concerns.
Learn more about virtual second opinions.
Locations
Gynecologic oncology services are available at the following locations:
Clinical Trials
Clinical Trials
- To learn more about what clinical trials are.
- To see a listing of our gynecologic oncology trials.
- Contact our research line directly at 800.223.2273, ext. 58090 or 216.445.8090.