Granulomatosis with polyangiitis (GPA) is the new name for what used to be called Wegener’s granulomatosis. It’s an autoimmune disease that can affect your whole body, but especially affects your lungs and kidneys. Polyangiitis is chronic inflammation in your smaller blood vessels. Granulomatosis involves small masses forming in your blood vessels and other organs.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
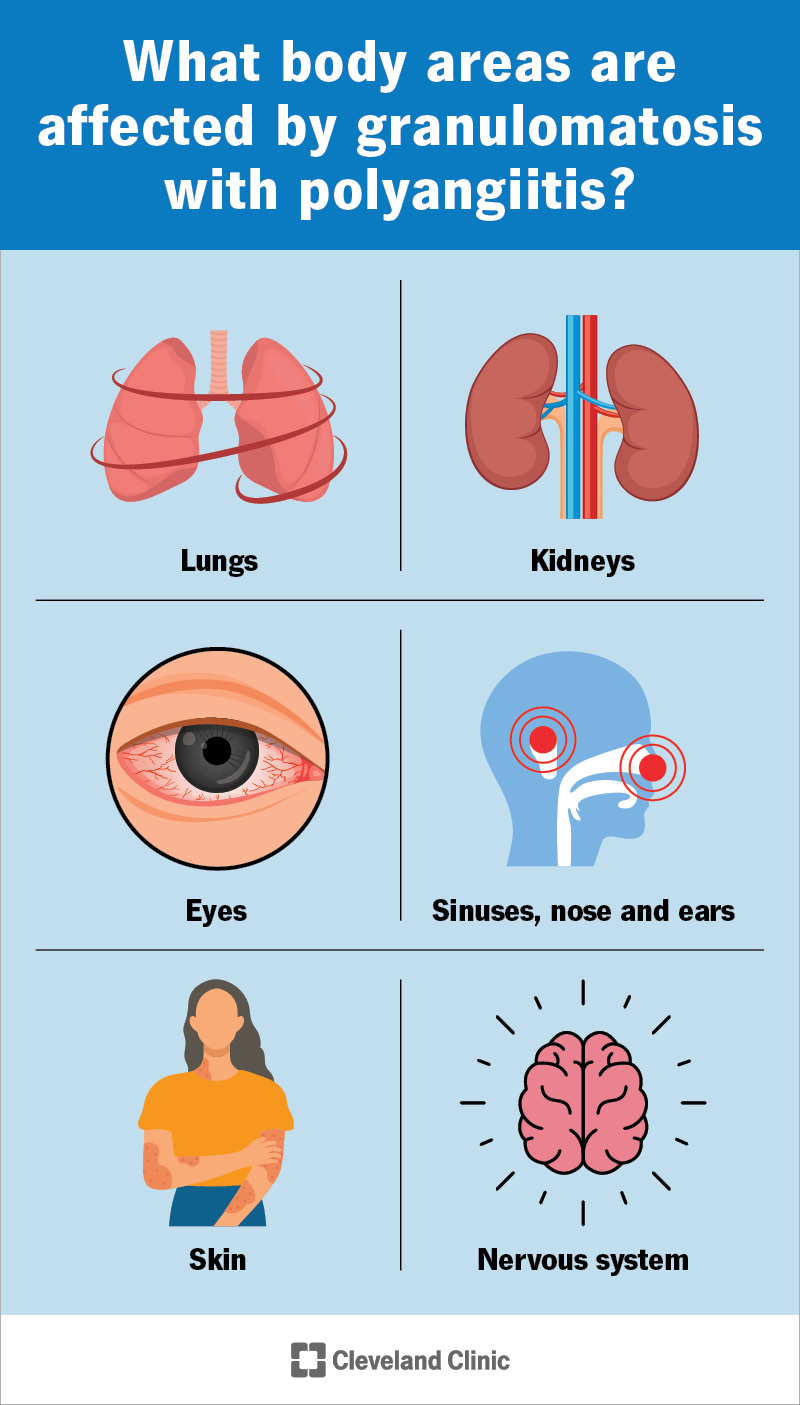
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/granulomatosis-polyangiitis-infographic)
Granulomatosis with polyangiitis (GPA) is a type of vasculitis — chronic inflammation in your blood vessels. It was formerly called Wegener’s granulomatosis, but the new name describes it more precisely. GPA involves:
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Different types of vasculitis affect different blood vessels. GPA affects the many smaller blood vessels throughout your body. This means it can cause issues throughout your body, but especially in organs that rely on many small blood vessels. GPA tends to affect your respiratory system and kidneys the most.
Inflammation in your blood vessels can cause them to swell, break and bleed. It can also cause scarring that restricts the blood flow through your vessels, depriving your tissues of oxygen and nutrients. GPA can cause bleeding and organ damage in your renal and pulmonary systems (pulmonary-renal syndrome).
GPA affects your respiratory system and kidneys the most. But it can also affect many other organs and tissues, and how you feel overall. The smaller blood vessels that it targets travel throughout your body.
Vasculitis in your connective tissues may cause muscle pain and joint pain, along with an overall feeling of unwellness (malaise). Other general symptoms may include fatigue, loss of appetite and weight loss.
Advertisement
Many people with GPA first notice and seek treatment for symptoms in their respiratory system. Early symptoms might resemble a cold or infection, but they linger too long. They might include:
As granulomatosis with polyangiitis worsens, you might develop inflammation of the cartilage in your ears, nose and throat (polychondritis). This can cause more severe symptoms, including:
You can also bleed in your lungs, which may cause shortness of breath or coughing up blood.
You may not experience kidney pain with GPA. But you may notice changes in your pee, like foamy pee or blood in your pee. Swelling in your face or feet (edema) is another symptom of kidney disease.
If you have GPA, healthcare providers will continue to check on your kidneys, even if you never develop symptoms. While kidneys aren’t always involved in GPA early on, they almost always are eventually.
GPA can affect your eyes, causing inflammation on the surface or the inner parts of your eye. This can cause eye pain and pressure and make your eyes red and swollen. Severe cases can lead to vision loss.
Vasculitis in your skin may show up as:
Granulomatosis with polyangiitis may affect your nervous system. It usually affects your peripheral nervous system — the nerves that extend from your spinal cord to the rest of your body.
Inflammation and swelling may compress or damage just one nerve, causing symptoms in just one area (mononeuropathy). More commonly, it may affect multiple nerves (polyneuropathy). Symptoms can include:
Severe GPA can be organ-threatening and life-threatening. Complications can include:
Advertisement
GPA, like other types of vasculitis, is an autoimmune disease. This means your immune system generates ongoing inflammation in your blood vessels. Normally, your immune system sends inflammation to target infections. But in autoimmune diseases, it targets your healthy tissues by mistake.
Researchers aren’t sure why autoimmune diseases occur. There are probably multiple factors involved. Sometimes, extra stress on your immune system seems to push it into overdrive, triggering dysfunction. Researchers have associated the onset of GPA with certain severe bacterial and viral infections.
Granulomatosis with polyangiitis (GPA) belongs to a group of conditions called ANCA-associated vasculitis, or AAV. These are types of vasculitis that involve a specific antibody called ANCA. Researchers believe this antibody plays a role in triggering the inflammation in these conditions, including GPA.
A healthcare provider will begin by asking about your symptoms and physically examining you. If your symptoms and medical history suggest GPA, they’ll follow up with tests to investigate further.
Tests for granulomatosis with polyangiitis include:
Advertisement
Healthcare providers treat granulomatosis with polyangiitis (Wegener’s) with anti-inflammatory and immune system-suppressing drugs (corticosteroids and other immunosuppressants).
Some of these medications are stronger than others. Which combination your provider prescribes will depend on how severe your condition is and how much you’re at risk of the side effects.
Initial treatment for active GPA includes:
If you have severe complications, you might need additional treatment, such as:
Once GPA is in remission, you’ll take milder medications to maintain remission. These typically include:
You’ll have ongoing testing during treatment to monitor your condition and response to the treatment. Your healthcare provider will adjust your prescription and dosage according to your response.
Advertisement
Each medication comes with its own potential side effects, and they can occur at any time during your treatment. You might need to change medications to avoid or reduce the risk of certain side effects.
Granulomatosis with polyangiitis is a lifelong condition that requires lifelong care. With treatment, the disease can go into remission and stop causing symptoms. But symptoms can also return (relapse).
You may have to take medications off and on for the rest of your life to manage relapses. Since these medications suppress your immune system, you’ll also have to take extra care to prevent getting sick.
With effective treatment, you can live a relatively normal life with GPA. Most people with chronic diseases have periods of remission and relapse, so the course of the disease can be up and down.
Without treatment, the average life expectancy is five months, with less than 50% surviving one year. But with treatment, follow-up studies show more than 80% of people are alive at least eight years later.
Before treatment, organ failure is the biggest mortality risk with GPA. During treatment, you’re more at risk of life-threatening infections that can take hold when your immune system is suppressed.
When you’re living with a chronic autoimmune disease like granulomatosis with polyangiitis, you need to maintain a certain awareness of your body. Even when you’re feeling well, you should live defensively.
Take steps to protect yourself from common illnesses while taking immunosuppressants. Make sure to notice any new or unusual symptoms and let your healthcare provider know about them right away.
Granulomatosis with polyangiitis can affect you in many ways, some of which are life-threatening. Recognizing that something’s wrong and getting timely treatment for it can make all the difference.
With treatment, most people can live without symptoms at least some of the time. But your healthcare team will continue to monitor your condition. They’ll be your lifelong partners in maintaining your health.

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s primary care providers offer lifelong medical care. From sinus infections and high blood pressure to preventive screening, we’re here for you.
