Eye pain can affect one or both eyes. You can have eye pain because of things like injuries, inflammation and infections. Treatment depends on the cause of eye pain and may include things like eye drops, shielding your eyes or having surgery.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
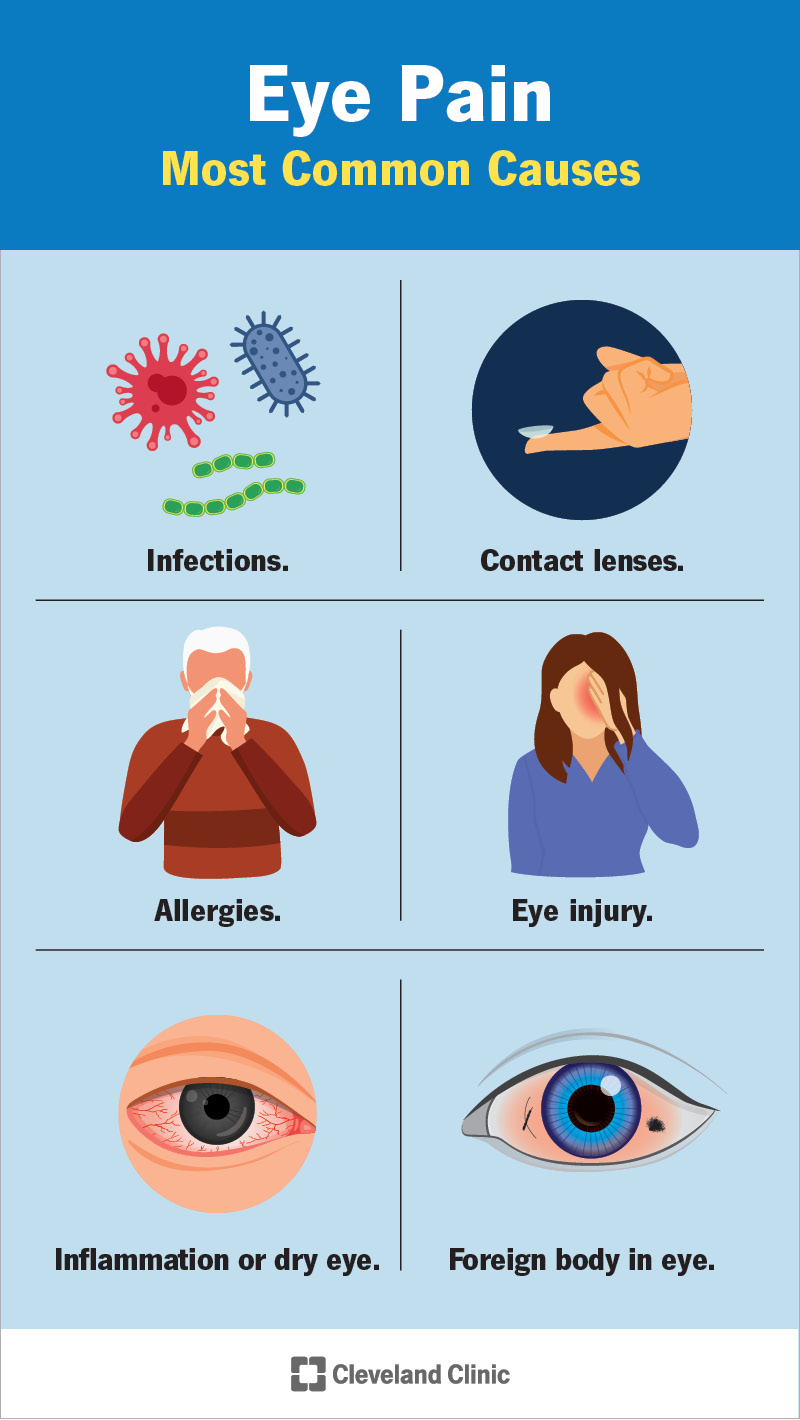
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/17796-eye-pain-infographic.jpg)
You may describe eye pain as sharp, aching or throbbing. It may happen in one eye or both eyes. You might also describe your eye pain in terms of where it hurts, like pain behind your eye.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Eye pain is more serious than the simple irritation you feel when you have a piece of dirt or an eyelash in your eye. Eye pain is more than the feeling of eyestrain that you might feel after staring at a computer all day. In those cases, your eye feels better when the lash or dirt is out of your eye or when you’re able to rest your eyes by closing them or using a cool compress.
The more serious type of eye pain is intense, lasts longer and can happen along with other symptoms. Sometimes eye pain can be a sign of an underlying health problem or injury. You should talk to a healthcare provider as soon as you can if you have a new eye pain or eye pain that keeps getting worse.
Eye pain due to injuries can happen to anyone, particularly if you don’t wear protective eyewear during activities that put your eyes at risk.
You may be more prone to eye pain if you wear contact lenses or if you have certain conditions, like allergies or sinus issues.
Eye pain can refer to pain in almost any part of your eyes, including:
Advertisement
Being able to explain where your eye hurts can help your healthcare provider determine the cause.
In most cases, a provider will start by asking you about your medical history and your symptoms. They’ll probably ask you:
A provider will also do a complete eye exam. They’ll use microscopes and other equipment to examine the eye. It’s possible the provider will also use drops to dilate your pupils for a thorough evaluation.
Many conditions and factors can cause eye pain. These can include:
People describe eye pain in different ways, including feeling like:
Common conditions, signs and symptoms linked to eye pain can involve only one part of the eye or more than one part. Many types of eye problems can cause pain, including the following conditions.
Advertisement
The first step to treating eye pain is generally to determine the cause and then treat that cause. You may not need pain medications.
Treating eye pain that results from infections may include:
You can help yourself when you have eye pain and infection by:
If you have an eye injury, you should follow these tips:
Advertisement
You might wonder when you should be concerned about eye pain. You should take any case of eye pain seriously. However, if you have eye pain along with any of the following symptoms, you should get medical help quickly:
If you injure your eye, or you have intense eye pain, the best thing to do is to go to an emergency room or contact a healthcare provider right away. A provider can make a diagnosis by doing an examination and asking questions about your symptoms. In cases where eye pain happens because of an underlying medical condition, it’s necessary to treat the condition to find relief for your eye pain.
Advertisement

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s ophthalmologists and optometrists have the highest training available. We provide exams, vision correction and care for many eye conditions.
