Prostatitis is a group of conditions that includes acute and chronic bacterial prostatitis and chronic pelvic pain syndrome (CPPS). It can cause infection, inflammation and pain in the prostate gland. Asymptomatic inflammatory prostatitis doesn’t causesymptoms. Acute (sudden) prostatitis is a medical emergency.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
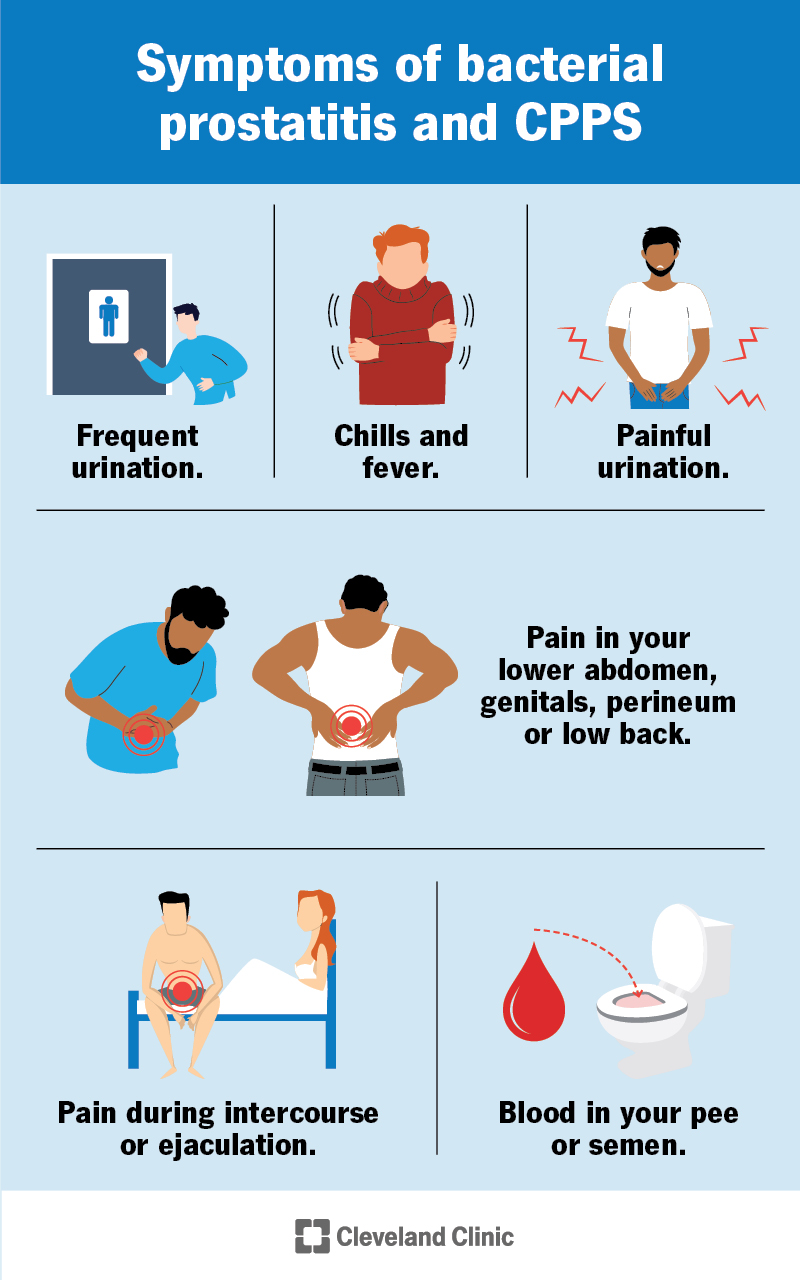
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/15319-prostatitis)
Prostatitis is inflammation of your prostate gland. Your prostate gland sits below your bladder, in front of your rectum. Your urethra (the tube that carries pee and semen out of your body) runs through the center of your prostate.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
If you have one of the four types of prostatitis, the tissue in and around your prostate gland becomes swollen, tender and irritated. Urinary tract infections (UTIs) and other bacterial infections can cause certain types of prostatitis, but some have no cause. There are treatments that help manage your symptoms.
Types of prostatitis include:
Advertisement
More than 2 million men see a healthcare provider every year for prostatitis symptoms. Up to 50% of men will have symptoms of prostatitis at some point in their lives. It’s the most common urinary tract issue in people men under 50 and the third most common in men over 50.
Prostatitis symptoms vary depending on the type and cause. It’s important to see a healthcare provider if you feel pain in your pelvis or experience urination changes.
People with nonbacterial prostatitis may not have any symptoms. The other three types of prostatitis share symptoms, such as:
Acute bacterial prostatitis causes flu-like symptoms like fever, body aches and chills.
Different types of prostatitis have different causes. Sometimes the cause isn’t known and other times it’s clear that the cause is a bacterial infection.
Potential contributors to chronic pelvic pain syndrome or CPPS include:
It’s important to note that bacteria don’t cause CPPS or nonbacterial prostatitis.
The bacterial forms of prostatitis happen as a result of a bacterial infection. Bacteria can get in your prostate through your urethra or when your urine flows backward (vesicoureteral reflux).
Potential causes of bacterial forms of prostatitis include:
Some risk factors for bacterial prostatitis may include:
People with nerve damage or trauma to their pelvises may be more at risk of chronic pelvic pain syndrome.
Being older than 50 and having a condition like enlarged prostate (benign prostatic hyperplasia) also increases your risk for all types of prostatitis.
People with acute bacterial prostatitis may develop sepsis. This is a life-threatening, widespread infection in your body. It requires immediate medical treatment. Other complications could include:
Advertisement
Prostatitis is benign (not cancerous). It doesn’t increase your risk of prostate cancer. But, inflammation from prostatitis sometimes raises the level of prostate-specific antigens (PSA) in your blood — just like prostate cancer does. Further tests can help determine what’s causing elevated PSA levels.
Your healthcare provider will assess your symptoms and do a physical exam.
Less invasive tests for prostatitis may include:
More invasive tests for prostatitis include:
Advertisement
Prostatitis treatments vary depending on the cause and type. Nonbacterial prostatitis doesn’t require treatment.
For chronic pelvic pain syndrome (CPPS), your healthcare provider may use a system called UPOINT to classify symptoms into six categories. Your provider uses multiple treatments at the same time to treat only the symptoms you’re experiencing.
Approximately 80% of people with CPPS improve with the UPOINT system. The system focuses on these symptoms and treatments:
Advertisement
Antibiotics can kill bacteria that cause bacterial types of prostatitis. People with acute bacterial prostatitis may need 14 to 30 days of antibiotics. Some people need antibiotics through an IV (into your vein) in a hospital. Surgery to drain an abscess on your prostate may be necessary, but this is rare.
Treating chronic bacterial prostatitis is more challenging. Most people need between four and 12 weeks of antibiotics. If this approach doesn’t work and your symptoms come back, your provider may prescribe a low-dose antibiotic to prevent recurrent infection.
You should always see a healthcare provider before you treat prostatitis on your own at home. But they may recommend additional treatment you can do at home to manage your symptoms. This could include:
If a bacterial infection is causing prostatitis, it won’t go away on its own. You need medication to get rid of the infection. But, if you have CPPS or nonbacterial prostatitis, the inflammation and tenderness may subside without medication. Your healthcare provider can let you know what to expect based on your symptoms.
Drinking extra fluids can help you pee more often, which removes bacteria from your body. But you shouldn’t drink extra water as a substitute for getting medical treatment. Your healthcare provider will recommend how much extra fluid you should drink each day if you have prostatitis.
Staying hydrated is good for not only your prostate health but your overall health. Drinks like water, green tea and noncaffeinated drinks are good choices to maintain hydration. If you have specific questions about what food and drinks you should consume after a prostatitis diagnosis, you should check with your healthcare provider.
While it can cause unpleasant symptoms, the good news about prostatitis is that you usually feel relief with the right treatment. It’s not normal to feel pain in and around your rectum and genitals, or to experience changes in how you pee. You should always seek care for these types of symptoms.
Antibiotics treat most cases of bacterial prostatitis. While more challenging to treat, most people with CPPS feel better after receiving treatment for their symptoms using the UPOINT system. If you don’t feel relief with treatment, work with your provider until you do. They can make sure prostatitis doesn’t affect your quality of life.
Prompt treatment for UTIs may keep an infection from spreading to your prostate. If you’re sexually active, use a condom during every sexual encounter. Having safe sex can prevent prostatitis that results from STIs.
See a healthcare provider if you have pain in your perineum or experience changes to how you typically urinate. If you have prostatitis, this can prevent it from getting worse.
You should call your healthcare provider if you experience:
You may want to ask your healthcare provider:
Prostatitis is a common, and sometimes painful, condition that can affect men at any adult age. Unfortunately, there’s a lot of confusion about the disease because there can be many causes and types. There isn’t a one-size-fits-all treatment for prostatitis. That’s why it’s important to find out which type you have and follow your healthcare provider’s treatment plan.
Learn more about the Health Library and our editorial process.
Cleveland Clinic's health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability, and up-to-date clinical standards.
Cleveland Clinic's health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability, and up-to-date clinical standards.
You shouldn’t have a hard time peeing. Or have chronic pelvic pain. Cleveland Clinic’s expert providers can treat your prostatitis and help you get relief.
