Hepatocellular carcinoma (HCC) is cancer in your liver. Although it can be life-threatening, catching it early can mean successful treatment with surgery or a liver transplant. Other treatments ease your symptoms and help you live longer. If you’re at high risk for HCC, you should see your provider regularly to check for signs of HCC.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
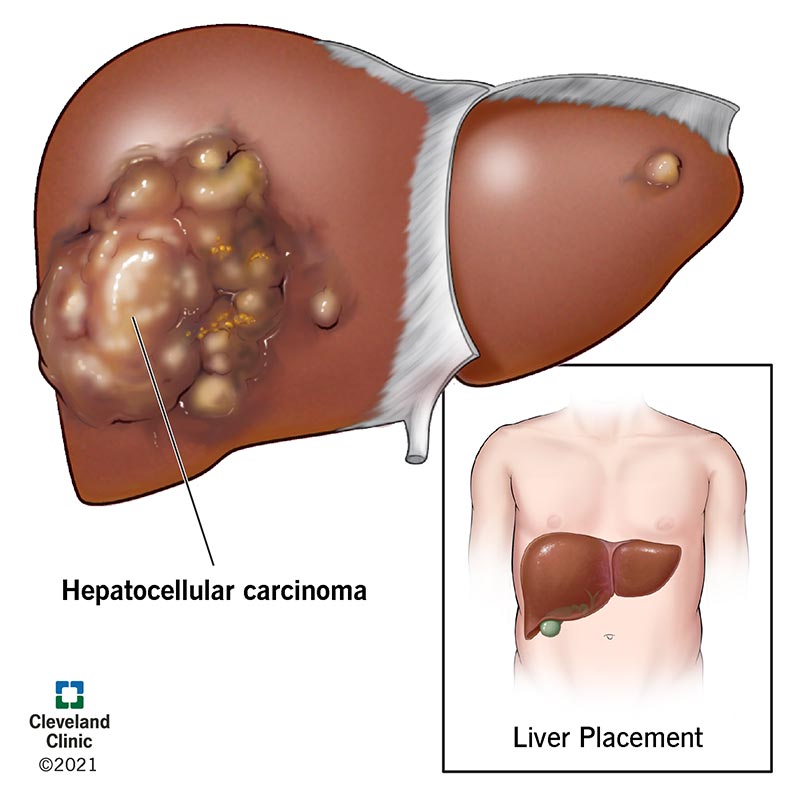
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/Images/org/health/articles/21709-Hepatocellular-Carcinoma-Illustration)
Hepatocellular carcinoma is the most common form of liver cancer. It’s an aggressive (fast-growing) cancer most common in people with advanced liver disease, like cirrhosis of the liver. Increasingly, people diagnosed with HCC have a liver condition that sometimes leads to cirrhosis called metabolic dysfunction-associated steatotic liver disease (MASLD).
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
In the beginning, hepatocellular carcinoma grows slowly. Surgery to remove the tumor or a liver transplant can treat HCC in its early stages. But most people don’t learn they have it until it’s advanced and spreading more quickly. Eventually, it can lead to liver failure. At this point, HCC is challenging for providers to treat.
Given how serious it is, you should receive regular checks for signs of HCC if you have cirrhosis or MASLD.
HCC accounts for about 85% to 90% of all primary liver cancers. “Primary” means the cancer starts in your liver (as opposed to spreading to your liver, as with metastatic cancer). It’s the sixth most common type of cancer diagnosis and the third leading cause of cancer-related deaths.
HCC is two to three times more common in men. Most people diagnosed are 60 or older.
Tumors may not cause symptoms in the early stages. But as HCC progresses, you may notice:
Advertisement
Many conditions cause similar symptoms, and most aren’t as serious as hepatocellular cancer. So, try not to panic if you experience one or more of them. But if symptoms last longer than two weeks, it’s best to see a healthcare provider.
Most people diagnosed with HCC have cirrhosis of the liver (approximately 80%) although some have a a condition that can lead to cirrhosis of the liver. In some instances, the condition never progresses to cirrhosis, but people still develop HCC.
With these conditions, unmanaged long-term liver inflammation can lead to severe scarring and, eventually, HCC.
Conditions that increase your risk of HCC include:
If you belong to a high-risk group, your healthcare provider may suggest regular screenings to catch HCC early, when it’s treatable. They can also help you take steps to reduce risk factors, like helping you quit smoking or drinking. They can help you manage chronic conditions that put you at risk, like hepatitis infections and diabetes.
Your healthcare provider will do a physical exam. They’ll also ask about your medical history, symptoms and lifestyle.
Tests to help confirm a diagnosis include:
HCC is an unusual cancer because in people with cirrhosis, providers can make the diagnosis based on the tumor(s) having certain features on an MRI or CT scan without needing to do a biopsy.
Advertisement
Cancer staging for HCC allows your healthcare provider to determine how advanced it is. It also helps them plan treatments and determine your prognosis (outlook). To stage HCC, providers consider:
Treatments include:
Advertisement
Your healthcare provider may suggest participating in a clinical trial to try new HCC treatments. They may also recommend palliative care to help you manage cancer symptoms and treatment side effects. Palliative care can improve your experience whether you’re living with long-term disease or receiving treatment for early-stage, curable HCC.
Surgery to remove the tumor or a liver transplant are the best options for a cure. If surgery isn’t an option, there are other treatments to ease your symptoms, slow the tumor’s growth and help you live longer.
Researchers continue to search for new ways to cure hepatocellular carcinoma that can’t be removed with surgery. In the meantime, new treatments, like immunotherapy and targeted therapy, continue to improve the life expectancy of people diagnosed with advanced HCC.
The five-year relative survival rate (people alive five years after their diagnosis) for people with HCC is 21%.
But many factors contribute to life expectancy, including how advanced HCC is, your liver’s overall health and your response to treatment. Some studies show that receiving care in a hospital that commonly treats HCC can improve survival rates.
Every case of HCC is different. Your healthcare provider is your best resource for offering insight into what you might expect based on your condition.
Advertisement
There are several ways you can reduce your risk of developing HCC. You can:
HCC can feel like an overwhelming diagnosis. It’s completely normal to feel uncertain about what happens next. But there are steps you can take to cope with your diagnosis and advocate for yourself.
You can:
Contact your provider if you have symptoms of HCC for two or more weeks or if existing symptoms get worse. Don’t skip check-ups if you belong to a high-risk group and your healthcare provider recommends screenings for HCC.
Catching HCC early, when surgery can treat it, delivers the best possible outcomes.
You’ll likely have several questions throughout your diagnosis and treatment. Don’t hesitate to ask any questions you have about your diagnosis, treatment or likely outcomes.
Questions to ask include:
There isn’t an ideal way to cope with a serious condition like hepatocellular carcinoma (HCC). It’s completely normal to feel overwhelmed, anxious and even afraid. But there are steps you can take to help yourself as you prepare for what comes next. To feel more confident about your choices, take time to understand your treatment options and side effects. To avoid feeling isolated, share your experience with others going through the same thing. HCC is a difficult diagnosis to receive, but you don’t have to go it alone.

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Getting liver cancer treatment at Cleveland Clinic means you’ll get multidisciplinary care with advanced testing, procedures and therapies that aren’t widely available.
