Your popliteal artery travels from your lower thigh to your upper calf, behind your knee. It’s a continuation of your femoral artery and a key supplier of oxygen-rich blood to your knee, calf and foot. Plaque buildup, traumatic injuries and other conditions can limit or block blood flow in your popliteal artery, requiring treatment.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
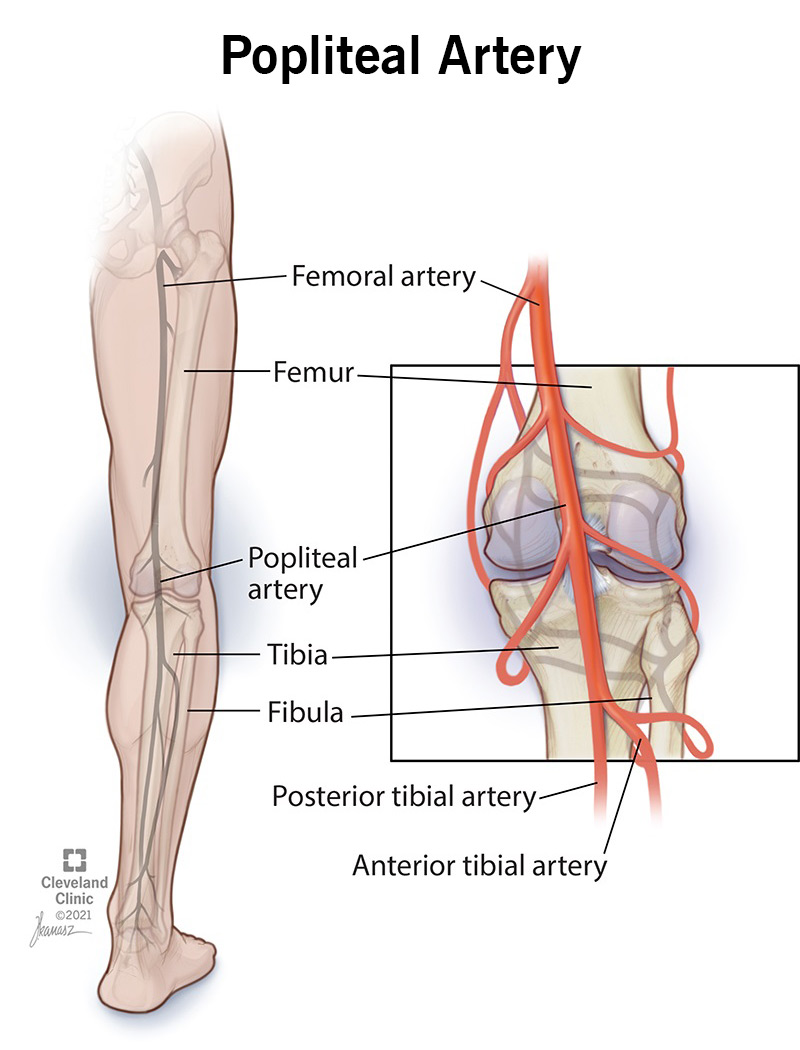
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/22708-popliteal-artery)
Your popliteal artery is a blood vessel that runs down the back of your knee. You have one in each leg. Together with their branches, your popliteal arteries deliver blood to your knees, lower legs and feet.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Your popliteal arteries support healthy blood flow in your lower body. Each popliteal artery has many branches that extend above, below and around your knee. This network of arteries delivers oxygen-rich blood to your:
Your popliteal artery also serves as a pulse point. Your healthcare provider may press on it to see how well blood is flowing in your leg.
Your popliteal artery is behind your knee. It starts in your lower thigh as a continuation of your superficial femoral artery. The exact spot where it begins is in a space between your muscles called the adductor canal.
From the adductor canal, your popliteal artery travels down through the popliteal fossa. You might hear this called your “knee pit.” It’s the soft spot behind your knee. Blood vessels and nerves pass through this area.
After crossing through the popliteal fossa, your popliteal artery ends just below your knee in your upper calf. There, it splits into two terminal (end-point) branches:
These arteries get their blood supply from the popliteal artery. They send that blood on to your ankle and foot.
Advertisement
Besides its terminal branches, your popliteal artery has other branches along its course. These branches extend from the artery in your knee area. Picture a main road with side streets that intersect with it. The “side streets” that branch from your popliteal artery include your:
Traumatic injuries, plaque buildup and other health conditions can limit or block blood flow in your popliteal arteries. This can keep your legs and feet from getting the blood and oxygen they need to work as they should. In severe cases and without treatment, popliteal artery damage can lead to limb loss.
Examples of conditions that can affect your popliteal artery include:
Call your provider if you have:
These lifestyle changes can keep your arteries and circulatory system healthy:
Your popliteal vein is a blood vessel that runs just behind your popliteal artery, with blood flow going the opposite way. Your popliteal artery carries blood that’s rich in oxygen to your tissues. By contrast, your popliteal vein carries blood that’s now low in oxygen. The vein drains this blood from your feet, calf and knee area and sends it back up toward your heart.
When your leg is slightly bent, touch the soft spot behind your knee. That’s where your popliteal artery is located. Unlike your veins, it’s not visible through your skin. But it’s there, working hard to keep blood moving down your leg.
If you have a condition that affects this artery, your healthcare provider can help. They’ll explain your treatment options and let you know what you can expect. Make sure to ask any questions you have. Follow up with your provider anytime you have new or changing symptoms.
Advertisement

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s primary care providers offer lifelong medical care. From sinus infections and high blood pressure to preventive screening, we’re here for you.
