Claudication is muscle pain that happens when you’re active and stops when you rest. People usually describe it as cramping, aching, tingling or numbness in your lower body. Most cases happen because of a shortage of oxygen from circulatory problems like peripheral artery disease. Early diagnosis and treatment lead to better outcomes.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
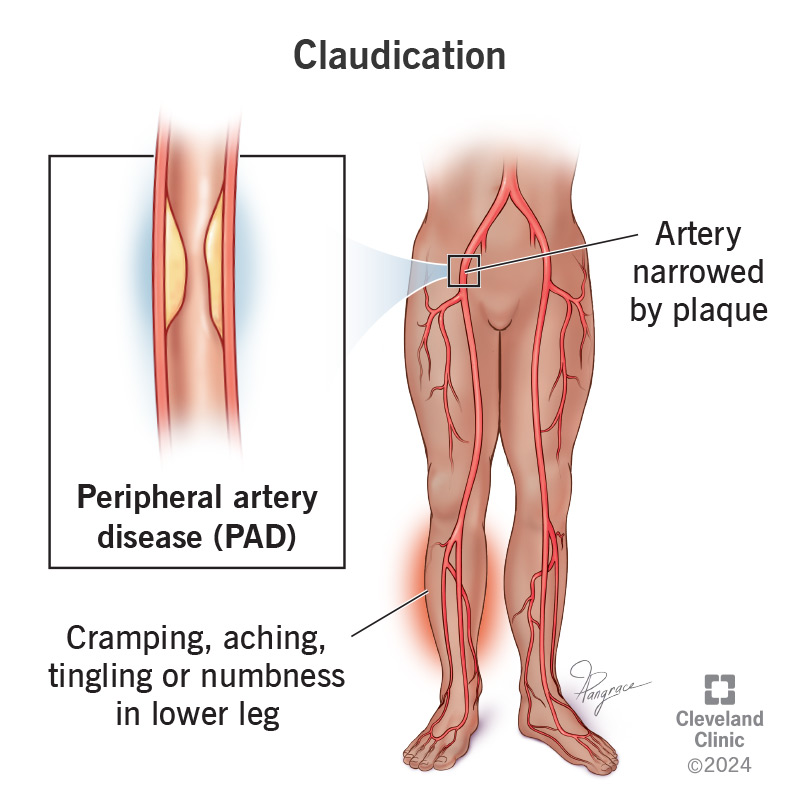
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/21972-claudication)
Claudication is the name for muscle pain that happens when you’re active and stops when you rest. This usually happens in your legs. You may be walking along and have to stop. But the pain gets better when you stand still for two to five minutes. Vascular claudication is usually a symptom of serious blood flow problems, especially peripheral artery disease (PAD).
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Vascular claudication may lead to critical limb ischemia. This is a severe blockage in a leg or arm artery. But there’s hope. Claudication treatments of various types can lower your risk of damaging a limb.
Another type, neurogenic claudication, comes from problems with your spine and nervous system.
Some people don’t have claudication symptoms. People who do may have these issues with their legs or feet:
Claudication is a classic symptom of peripheral artery disease (a narrowing of the blood vessels in your legs) and atherosclerosis (hardening of the arteries). Peripheral artery disease and atherosclerosis increase your risk of heart attack and stroke.
Claudication causes include circulation issues that keep your body from getting the amount of oxygen it needs. All the cells in your body need oxygen to function. When you’re more active, even just for a short walk, the cells in your muscles need more oxygen.
When people with poor circulation are more active, they feel pain. This is because their muscles need more oxygen than their body can provide. This type of pain is most common in your legs, but can also happen in your arms.
Advertisement
The pain goes away when you rest because your circulation can keep up with the lower oxygen demand. Claudication is also a concern because the pain it causes when walking often keeps people from being active. Stopping physical activity only makes the claudication worse.
Your risk of developing claudication goes up as you get older. The following factors can increase your risk of developing claudication:
To find out if you have claudication — or how severe your case is — your healthcare provider will perform a physical exam. They’ll examine your legs and feet, looking for color changes, wounds that are slow to heal or any other signs of poor circulation. They’ll also feel for your pulse in your legs and feet.
A provider may order these tests to diagnose claudication:
Claudication treatment can start with things you can do yourself. If your case becomes more severe, you may need medicine or a procedure. Treating claudication is important because it usually means you have peripheral artery disease or another circulatory disease that can be life-changing and even deadly.
Your provider may encourage you to quit using tobacco, eat heart-healthy foods and walk more. Walking is the best type of physical activity for claudication. This improves your blood flow by opening your blood vessels wider.
Providers recommend walking for 50 minutes three to five times a week. You’ll need to stop to rest when your legs hurt and then start again. The 50-minute goal includes rest breaks. Little by little, you can increase the time you spend walking. Taking walks regularly can help you walk farther and faster in a month or two.
Your provider may prescribe medications that:
If medicines don’t work, your provider may want to do a minimally invasive treatment. They may use angioplasty to treat a narrow or blocked artery by using a catheter. A provider may also put a stent into an artery they open to help it stay that way. Another option is bypass surgery to reroute blood flow. Providers only use surgery in severe cases.
Advertisement
Claudication won’t go away by itself. You’ll need some level of treatment to manage it. You can expect to have regular checkups with your provider so they can see how you’re doing. This is especially true if you’ve had bypass surgery to improve blood flow in your legs.
Treatment for claudication gives many people a good prognosis (outlook). But it’s important to remember that peripheral artery disease (which causes claudication) is a lifelong condition. PAD progresses faster in some people than others. The expected length of your life depends on your specific situation. This includes any other diseases you have.
Yes. There are many things you can do to prevent vascular claudication or delay its onset. You can:
You can care for yourself by following your provider’s instructions for treating claudication. Leg pain can come back if you stop taking walks. And claudication can get worse with tobacco use.
If you have claudication, your healthcare provider will want to know about it because it’s a key symptom of peripheral artery disease. Early diagnosis and treatment can prevent or delay the worsening of claudication symptoms to the point where they impact your life. You should also talk to your provider as soon as possible if this symptom develops or worsens suddenly.
Advertisement
Even if you don’t have any other health issues, it’s still important to talk to your provider about claudication. This is because it can be a sign of other diseases and conditions. Most of these conditions are serious and some of them are medical emergencies. These include:
Chronic compartment syndrome
Muscle groups, including their related nerves and blood vessels, are part of a “compartment.” A membrane called “fascia” (pronounced “fash-ia”) contains this compartment. If the tissue inside a compartment swells, the fascia compresses what’s inside the compartment, limiting blood flow and causing pain. Chronic compartment syndrome isn’t usually an emergency.
Deep vein thrombosis
Deep vein thrombosis (DVT) happens when a blood clot forms in a vein (typically a vein in your leg). If a clot breaks free and travels to your lungs, it can get stuck and block blood flow. This is a life-threatening medical emergency called pulmonary embolism.
Popliteal artery entrapment syndrome (PAES)
PAES is a rare condition that happens when a muscle defect compresses an artery in your leg, cutting off blood farther down. PAES can be a medical emergency in more severe cases. You’ll likely need surgery to fix this.
Advertisement
Questions to consider asking your provider may include:
Being unable to walk as much as you used to is frustrating. But walking is the best medicine for people with claudication. Ask your provider for a structured plan you can do at home or a supervised plan away from home. With either option, you have the power to improve your situation.

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Plaque in your blood vessels can cause tingling, pain and numbness. Cleveland Clinic’s experts treat circulatory problems, including peripheral artery disease.
