Time in range (TIR) is a measurement people with diabetes and healthcare providers use to assess their diabetes management. It’s most efficient to calculate your TIR with the use of a CGM. There are general guidelines for TIR goals, but you may have different goals based on your unique situation.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
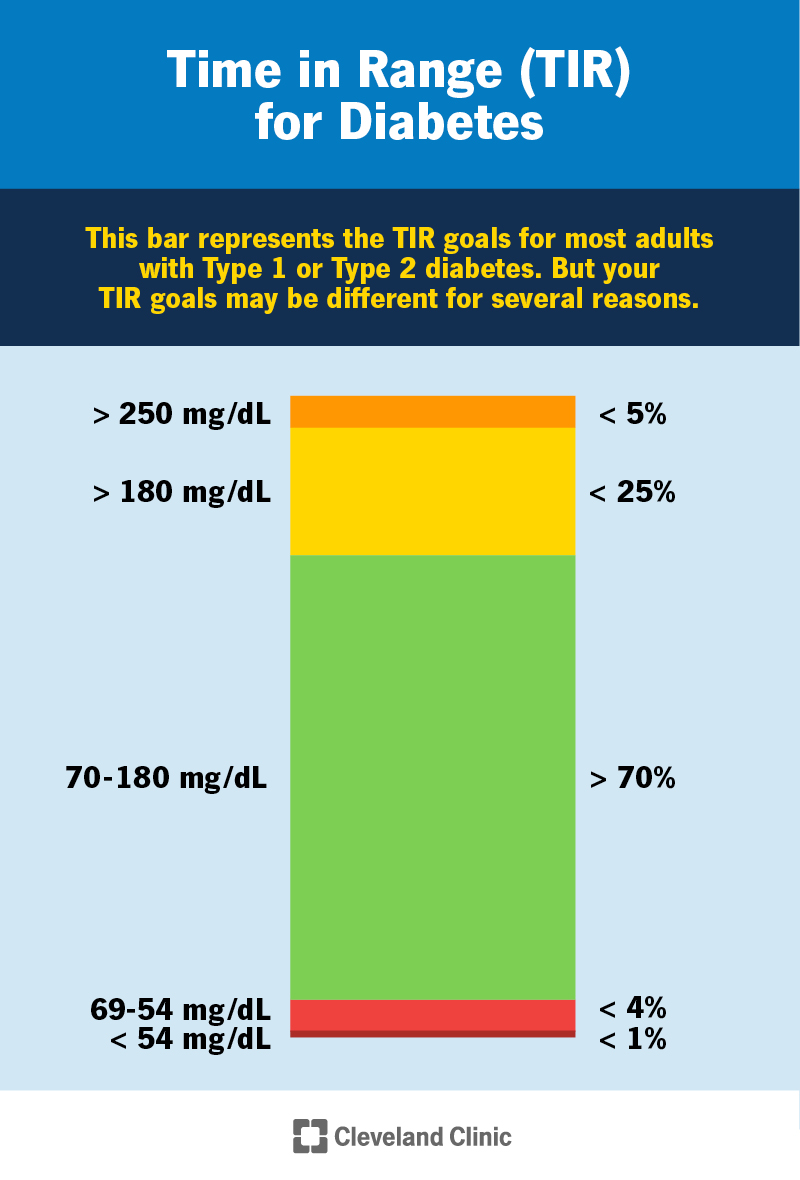
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/time-in-range-diabetes)
Time in range (TIR) is the amount of time a person with diabetes spends in a target glucose (sugar) range. For most — but not all — adults with Type 1 or Type 2 diabetes, that’s between 70 and 180 mg/dL. TIR is measured as a percentage. Healthcare providers typically recommend aiming to have a TIR above 70% (at least 17 hours of a 24-hour day).
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
It’s easiest — and most accurate — to calculate your time in range using a continuous glucose monitor (CGM). A CGM is a wearable technology that tracks your glucose levels over time. It measures the glucose level in the interstitial fluid just under your skin 24 hours a day while you’re wearing the device. CGMs allow you to download glucose data with software or an app to learn your time in range for a given period.
You can also use manual finger prick checks to calculate your TIR. But you’d have to check your blood sugar several times a day to get a more accurate picture of your TIR. A CGM provides more glucose data than manual finger pricks.
With CGMs, more and more people with diabetes — and their healthcare providers — are using TIR to better assess how their diabetes management is going. Looking at TIR data can help you and your provider set goals and make changes to your management plan.
Software programs for CGMs most often present time in range information as a color-coded vertical bar. The bar will show the percentage of time you’re in various ranges. The in-range section is typically green, and other ranges may be different shades of yellow, orange or red. From bottom to top, here are the ranges most standard CGM reports use:
Advertisement
CGM reports may show these data in other ways. Talk to your healthcare provider if you have questions about interpreting the information.
If you have diabetes, your target range for glucose levels is unique to you. Together, you and your healthcare provider will decide the target range that’s ideal for you and what percentage of time you should aim to be in-range. This will likely change throughout your life.
Glucose targets vary based on:
In general, TIR goals for most adults with Type 1 or Type 2 diabetes are:
In general, TIR goals for people who are at a higher-than-average risk for hypoglycemia (low blood sugar) are:
In general, TIR goals for adults with Type 1 diabetes in pregnancy are:
Guidelines for gestational diabetes and Type 2 diabetes during pregnancy may be different. Again, it’s important to discuss the most beneficial — and realistic — glucose goals for you with your healthcare provider. These are just general guidelines.
Time in range (TIR) measures your range of glucose levels over a period of hours to days. It depends on how long and frequently you wear your CGM and what period of time you want to check. In comparison, A1C (a laboratory blood test) measures your average glucose over the past eight to 12 weeks. An A1C test can’t give you information on blood sugar fluctuations. In general, researchers have found that as your TIR increases, your A1C typically decreases. But it isn’t an exact science.
You can think of A1C as reading a summary of a chapter of a book. In comparison, using a CGM and reviewing TIR is like reading the entire chapter — you have a more nuanced understanding of it.
Advertisement
Since the 1960s, healthcare providers and people with diabetes have relied on A1C as the main way to gauge how well their overall management is going. More recently, with the invention of CGM devices, providers and people with diabetes have found time in range to be a more helpful and accurate representation of diabetes management.
For people with Type 1 diabetes in particular, blood sugar levels can fluctuate significantly throughout the days, weeks and months. Because of this, A1C isn’t always an accurate measurement of management since it’s based on an average.
For example, a person who has frequent blood sugar fluctuations between significantly low and high episodes may have an A1C of 7%. A person who has blood sugar levels that stay more consistently around 154 mg/dL may also have an A1C of 7%. The TIR between these two people would be different.
In addition, A1C can be inaccurate in people with:
The accuracy can vary among different racial and ethnic groups, as well.
At this point in time, TIR likely won’t replace the need or use for A1C tests. Countless studies over the decades have shown that A1C benchmarks can help predict your likelihood of developing or avoiding diabetes complications. Instead, providers use TIR and A1C tests together to see a more informed picture of glucose management.
Advertisement
Time in range gives you a more accurate look at the glucose fluctuations that come with diabetes. Countless factors can affect blood sugar levels — from food and physical activity to medications and your stress level. Reviewing your TIR data (and using a CGM) offers better insight into how certain factors directly affect your glucose levels.
For example, you may notice that your TIR was lower when you were sick with the flu for a week. Given that insight, you may want to ask your healthcare provider how to be more prepared to manage diabetes the next time you get sick.
Research is ongoing, but studies so far are finding links between lower time in range and an increased risk of diabetes-related complications.
Studies show that large glucose fluctuations (glycemic variability) may increase oxidative stress and inflammation. These issues may cause cell damage. Several studies so far have linked large glucose fluctuations with:
In addition, one study revealed that people with Type 2 diabetes with a lower TIR and higher glycemic variability had more advanced diabetes-related retinopathy. Another study found that lower TIR was significantly associated with more severe cardiovascular autonomic neuropathy.
Advertisement
So far, these studies reflect the importance of optimizing your time in range. As researchers gather more information, diabetes experts may adjust time in range goals in the future.
The main strategy behind improving your time in range involves pinpointing what’s affecting your glucose levels. This can take time. In fact, it may feel like a never-ending science experiment. Because of this, it’s important to focus on one factor at a time — and to be kind to yourself. If you notice your glucose level is elevated — or low — consistently at a certain time of day, focus in on your habits and activities during that time frame.
For example, you may notice that your glucose level consistently spikes (goes out of range) after breakfast. Examples of things to consider that may be causing these spikes include:
This is just one example. Diabetes is a very complex condition, and there are several strategies that may help you improve your time in range. As always, it’s best to work with a healthcare provider who specializes in diabetes, like an endocrinologist or a certified diabetes care and education specialist (CDCES), when you want to make changes to your management plan.
Time in range is the newest metric for gauging glucose management for people with diabetes. It can be overwhelming trying to take in and interpret TIR information and your glucose data. Know that your healthcare provider will be by your side to help you understand and use TIR to your advantage. Together, you can monitor how your TIR changes over time and adjust your management strategy along the way.

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Whether you’ve been living with diabetes for years or you’re newly diagnosed, you want experts you can trust. Our team at Cleveland Clinic is here to help.
