Rectal cancer happens when cancerous cells develop in your rectum. Symptoms include rectal bleeding or changes in how and when you poop. Having a biological family history of rectal cancer or certain inherited disorders increases your rectal cancer risk. Treatments include surgery to remove cancerous tumors, chemotherapy, radiation therapy and targeted therapy.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
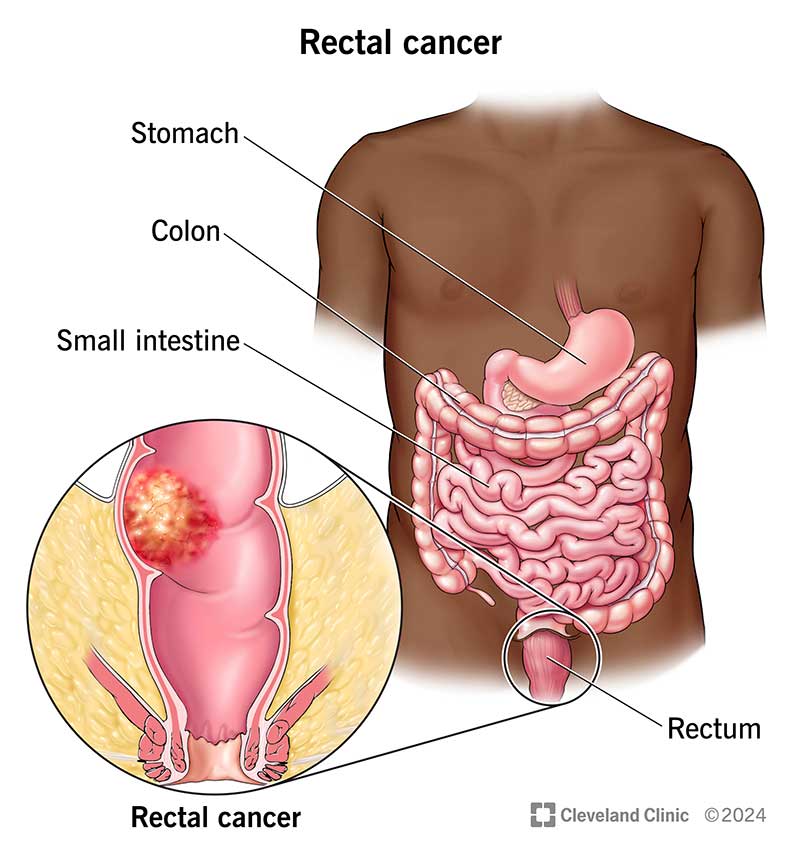
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/Images/org/health/articles/rectal-cancer)
Rectal cancer typically is a slow-growing cancer that forms on the inner lining of your rectum. Your rectum is the last several inches of your large intestine. Most rectal cancers start as clumps of abnormal cells (polyps) known as adenomas. It can take 10 to 15 years for a polyp to turn into a cancerous tumor on your rectum.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Cancer screening like colonoscopies often detect polyps that can become cancer. Regular screenings to detect and remove polyps reduce your risk of developing rectal cancer. If you have rectal cancer, surgery to remove small cancerous tumors may cure the condition.
Rectal cancer is the third most common cancer in your digestive system, behind colon cancer and pancreatic cancer. Experts estimate 46,200 people will receive a rectal cancer diagnosis in 2024.
You can have rectal cancer for years without noticing changes in your body. In many cases, rectal cancers don’t cause symptoms at all. However, some people may notice certain warning signs. Rectal cancer symptoms may include:
The exact cause of rectal cancer is unknown. But there are certain risk factors that increase your chance of developing the disease, including:
Advertisement
Diagnosis begins with routine screening tests, including digital rectal examination (DRE) and colonoscopy. Your provider may do a biopsy during your colonoscopy to obtain tissue samples for examination by a pathologist.
If lab tests detect cancer, your provider may refer you to an oncologist for additional tests. Those tests may include blood tests, imaging tests, procedures to confirm diagnosis, and lab tests for closer examination of cancerous cells in tissue samples.
Your oncologist may order the following blood tests to look for signs of rectal cancer:
Tests may include a diagnostic colonoscopy, which follows up on the test that detected abnormalities in your rectum. They may order a proctoscopy to look inside your rectum.
Your oncologist may order the following imaging tests to determine if cancer is spreading (metastasizing) from your rectum to other areas of your body:
Your oncologist will use test results to establish the cancer stage. Rectal cancer is categorized into five different stages:
Depending on your situation, your provider may do active surveillance. In active surveillance, sometimes known as watchful waiting, your provider carefully monitors your overall health and symptoms.
They may also do other treatments, including surgery. Surgery to remove cancerous tumors is one of the most common rectal cancer treatments. Your colorectal surgeon may consider several options, including:
Advertisement
Treatments other than surgery may include:
Surgery and other cancer treatments may cause several side effects. If you’re receiving rectal cancer treatment, you may want to consider palliative care. Palliative care is specialized care that can help you manage cancer symptoms, treatment side effects and other aspects of having a serious illness.
Clinical trials help healthcare providers and scientists find more effective treatments for different diseases. In a clinical trial, researchers intensively study treatment options for more effective ways to treat cancer. Ask your provider if a clinical trial is right for you.
Advertisement
Your prognosis, or what you can expect after treatment, depends on your situation. For example, if you had APR surgery, you may need to rely on a colostomy, which changes the way that you poop.
Overall, data from the National Cancer Institute (U.S.) (NCI) shows 68% of people with rectal cancer were alive five years after their diagnosis. The NCI groups cancer survival rates from tumor location instead of cancer stage. The five-year survival rates by tumor location are:
| Rectal cancer location | Five-year survival rate |
|---|---|
| Local: Cancer hasn’t spread outside of your rectum. | 91% |
| Regional: Cancer has spread outside of your rectum to nearby lymph nodes or to the lining of your abdomen (belly). | 74% |
| Distant: Cancer from your rectum is in your liver, lungs or distant lymph nodes. | 17% |
| Rectal cancer location | |
| Local: Cancer hasn’t spread outside of your rectum. | |
| Five-year survival rate | |
| 91% | |
| Regional: Cancer has spread outside of your rectum to nearby lymph nodes or to the lining of your abdomen (belly). | |
| Five-year survival rate | |
| 74% | |
| Distant: Cancer from your rectum is in your liver, lungs or distant lymph nodes. | |
| Five-year survival rate | |
| 17% |
While you can’t prevent rectal cancer altogether, there are steps you can take to reduce your risk. For example:
Regular cancer screening may reduce the chance that you’ll develop rectal cancer because screenings may detect precancerous polyps. And if you have rectal cancer, screenings may detect it while cancerous tumors are small and easier to treat. Colonoscopy is the most common screening test, but there are also other options:
Advertisement
In general, people age 45 and older should have regular colorectal cancer screening tests. Ask a healthcare provider or your primary care provider to recommend when you should have screening tests. A primary care provider knows you, your family medical history and your medical history and is your best source of information.
Your rectal cancer journey doesn’t end with treatment: Your oncology team may want to monitor your health for several years after you finish treatment. Living from test to test can be emotionally exhausting. If that’s your situation, consider participating in cancer survivorship programs.
Your follow-up appointments will vary depending on your situation, and may include the following timeline and tests:
If you’re undergoing rectal cancer treatment, call your healthcare provider right away if you develop:
If you’ve been diagnosed with rectal cancer, you’ll want to gather as much information as you can. Here are some questions to ask your healthcare provider:
Rectal cancer can cause symptoms that are hard to discuss, like changes in your poop. And screening tests for rectal cancer can be uncomfortable, starting with test preparation. But awkward conversations and uncomfortable tests may help your healthcare providers detect changes in your rectum that could become cancer. Tests may also find cancerous tumors before they grow and spread. Early treatment often leads to a cure. Talk to a healthcare provider if you have questions or concerns about rectal cancer. They’ll be glad to help you understand your personal risk for rectal cancer and recommend screening tests that make sense for you.
Learn more about the Health Library and our editorial process.
Cleveland Clinic's health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability, and up-to-date clinical standards.
Cleveland Clinic's health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability, and up-to-date clinical standards.
Colorectal cancer can turn your world upside down. At Cleveland Clinic, our experts will craft a treatment plan to help you get the best care possible.
