A flexible sigmoidoscopy is like a partial colonoscopy. It examines only the lower third of your large intestine. Your provider might suggest this procedure if you have unexplained symptoms related to your lower colon, rectum and anus.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
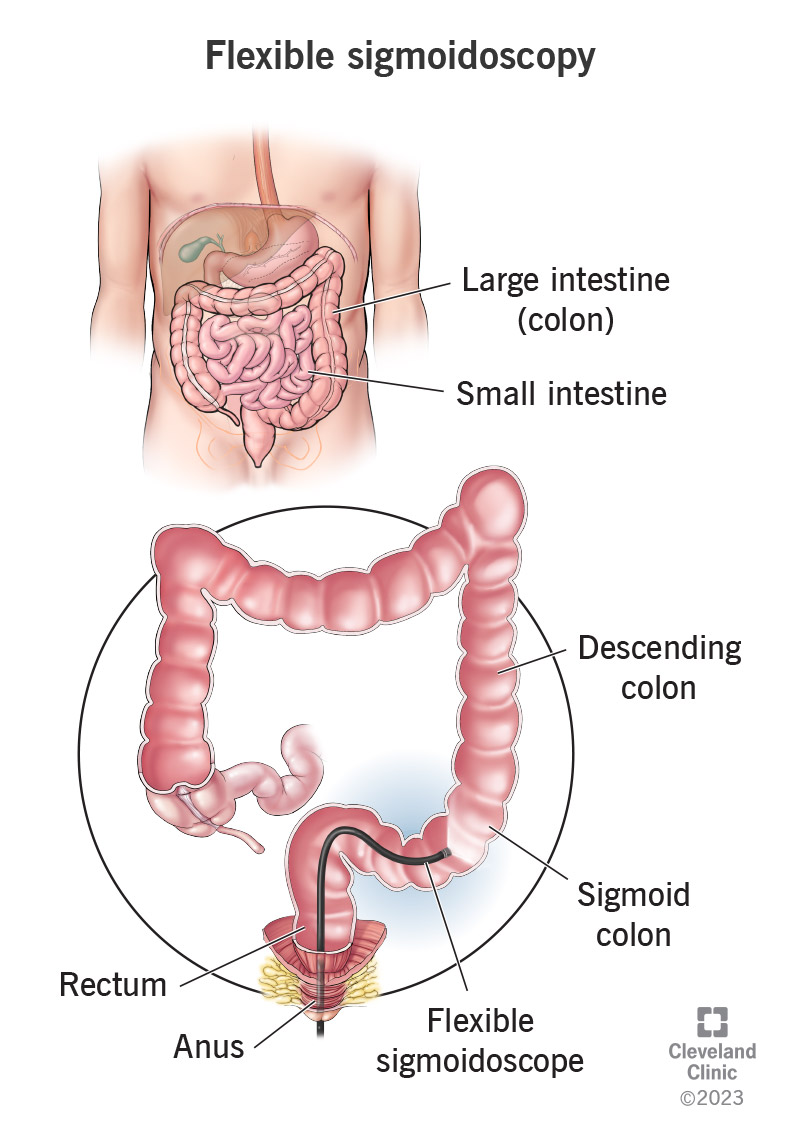
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/4953-flexible-sigmoidoscopy)
A flexible sigmoidoscopy is a procedure to examine the inside of your lower large intestine. A healthcare provider looks inside with a long, flexible tube with a camera attached (an endoscope). Different types of endoscopes have different names based on where they enter your body and what they examine. A flexible sigmoidoscope goes through your anus (butthole) and rectum to examine the lower third of your colon.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Your colon has four segments, the last of which is your sigmoid colon. The name, sigmoidoscopy, refers to this part of your colon. But the flexible sigmoidoscope actually goes a little further, into your descending colon. Your descending colon travels down the left side of your abdomen to meet your sigmoid colon, which curves inward toward the middle of your pelvis to meet your rectum.
Healthcare providers use flexible sigmoidoscopy to look for evidence of disease in your lower large intestine. The camera projects high-resolution images of your intestine to a screen so they can see in detail what’s going on in there. They can take tissue samples through the endoscope if needed, to test later in the lab (biopsy). Sometimes, they can even treat your condition through the endoscope.
You might have a flexible sigmoidoscopy to investigate unexplained symptoms, such as:
You might also have a flexible sigmoidoscopy to follow up on results from another test, like a blood test, stool test or imaging test. These tests can suggest certain conditions that might need to be investigated.
Advertisement
A flexible sigmoidoscopy might find:
Some people use flexible sigmoidoscopy along with other tests to screen for colorectal cancer.
A flexible sigmoidoscopy might find colorectal cancer in your lower colon or rectum. If it did, your healthcare provider would want to search the rest of your colon for cancer, too. This would require a colonoscopy. Since a flexible sigmoidoscopy doesn’t examine your entire large intestine, it’s not the most thorough screening tool for colorectal cancer. But for some people, it serves as a starting point.
If your symptoms or other test results seem to indicate that your condition is based in your lower large intestine, there might not be any need to look further. A colonoscopy is a more involved procedure than a flexible sigmoidoscopy and might be more difficult for certain people. It requires special preparation that a flexible sigmoidoscopy usually doesn’t require. It also may require sedation or anesthesia.
Some people choose to screen for colorectal cancer with more frequent sigmoidoscopies instead of colonoscopies. This is an option if you’re not at high risk for colorectal cancer and you have health factors that make a colonoscopy more difficult for you. Instead of a colonoscopy screening every 10 years, you can have a sigmoidoscopy every five to 10 years, along with a fecal occult blood test every year.
Most healthcare providers prefer that your bowels are relatively empty before a flexible sigmoidoscopy. This means they’ll want you to eat a restricted diet the day before the test and to take something to make you poop before the test. You won’t necessarily have to do the type of bowel prep that you’d do for a colonoscopy, but healthcare providers might ask this in some cases. They might prescribe:
Advertisement
Most people don’t need sedation or anesthesia for a flexible sigmoidoscopy, though you can discuss it with your provider if you’re anxious about it. The procedure isn’t painful, though you may feel some gas pain or cramping when the sigmoidoscope is advancing into your intestine. The sigmoidoscope blows carbon dioxide gas into your intestine to inflate it for better viewing. This will pass after the test.
Advertisement
It normally takes about 15 minutes. It might take a little longer if your provider needs to remove polyps or treat a wound. If they need to send tissue samples to the lab for testing, this will happen later.
Your provider will discuss what they found during the exam and any next steps. If they took biopsies, these results might take a few days to come back. You can return to your regular activities and diet.
There’s a low risk that the sigmoidoscope might injure your intestine or make it bleed. A little rectal bleeding is normal after the procedure, but it shouldn’t continue for more than a day. You might also have some leftover gas pain until the gas passes. Some people have diarrhea afterward. These are all temporary side effects. Walking around for a bit after the procedure may help them pass faster.
A rigid sigmoidoscopy uses a rigid scope rather than an endoscope. Instead of a long, flexible tube, it’s a shorter, unbending tube, about 25 cm long. A rigid sigmoidoscopy is also called a proctoscopy, and the tool is also called a proctoscope. “Procto” refers to your rectum. Although this scope goes as far as your sigmoid colon, it’s more often used to investigate symptoms related to your rectum and anus.
Advertisement
A flexible sigmoidoscopy is a quick, safe and efficient way for healthcare providers to diagnose and treat conditions in your lower large intestine. It doesn’t go as far into your body as a colonoscopy, so it doesn’t take as much time or preparation. It can be done with or without sedation. Most people tolerate it well without medication, even when they have tissue removed. Your provider might be able to find and fix your problem in one procedure.

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
A colonoscopy or other screening is an important test for colon cancer. The team at Cleveland Clinic can give you peace of mind and expert care when you need it.
