A colonoscopy is an examination of the inside of your large intestine (colon). It’s helpful for diagnosing gastrointestinal diseases, such as inflammatory bowel disease and colon cancer. It can also help treat and prevent colon cancer. Healthcare providers recommend routine colonoscopies for middle-aged and older adults to screen for cancer.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
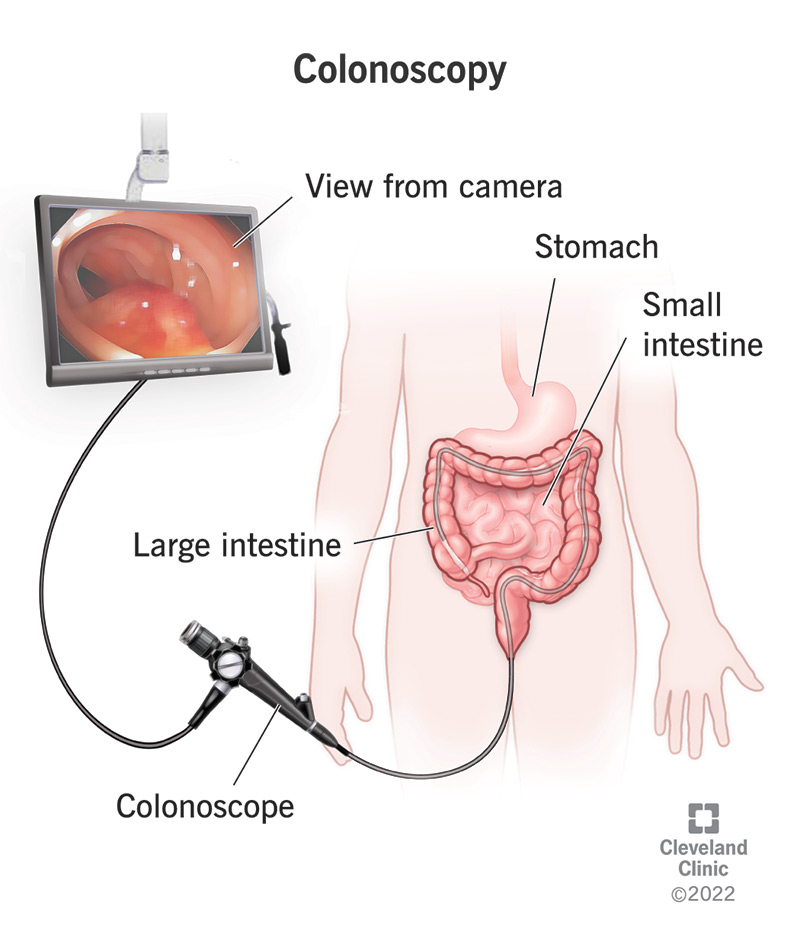
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/Images/org/health/articles/4949-colonoscopy)
A colonoscopy is an examination of the inside of your large intestine, which includes your colon, rectum and anus. It’s a type of endoscopy, which means that it uses an endoscope, a flexible tube with a lighted camera on the end that’s inserted into your body. There are different types of endoscopes for different parts of your body. In a colonoscopy, the colonoscope passes through your anus and rectum into your colon. Along the way, it sends pictures of the inside of your large intestine to a screen.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
A colonoscopy may be preventive, diagnostic or therapeutic — and often, it’s all of these. Your healthcare provider may advise you to have a colonoscopy for routine cancer screening if you’re at a statistically higher risk of developing colorectal cancer. Since anyone can have colorectal cancer at any time without warning or symptoms, screening is the best way to stay ahead of it. While screening, your gastroenterologist may also remove suspicious tissues for testing and prevention.
Most people will have their first colonoscopy for routine cancer screening. Statistically, your risk of developing colorectal cancer goes up as you age, which is why the American Cancer Society recommends regular screening at least by the age of 45. You may not have any reason to suspect you’re at risk of colorectal cancer, but when your statistical risk goes up, it’s best to check anyway. Colorectal cancer often doesn’t cause any symptoms until it’s too advanced to treat effectively.
You may be due for a colonoscopy for cancer screening if you:
Advertisement
If you have a primary care provider, or if you’re seeing a doctor for a checkup or treatment, ask them if you’re due for your routine colonoscopy screening. Based on your health history, they’ll be able to tell you when you should have one and refer you to someone who can give you one. In the United States, medical insurers and Medicare must cover routine colonoscopy screenings under the Patient Prevention and Affordable Care Act (PPACA). These screenings save thousands of lives each year.
Some people have colonoscopies because they have symptoms that a healthcare provider must investigate more closely. A colonoscopy provides a better view of your large intestine than other types of imaging tests that don’t go inside your body. Your doctor might need this better view to figure out what’s causing your symptoms or confirm their suspicions. Sometimes they might need to take a tissue sample (biopsy) to examine under a microscope in order to make a diagnosis. They can do that during the colonoscopy.
Symptoms that might require a colonoscopy include:
Diseases or conditions that a colonoscopy might help diagnose include:
One benefit of endoscopic procedures like colonoscopy is that if your endoscopist finds a problem during the procedure, they might be able to treat it at the same time. Endoscopists receive training to perform minor procedures with special tools that they pass through the endoscope. During a colonoscopy, they commonly remove any polyps (abnormal growths) that they find and test them for cancer. Removing polyps also prevents possible cancer from developing or spreading.
During your colonoscopy, the endoscopist can:
Colonoscopy prep is very important to the success of the procedure. Your healthcare provider will give you detailed instructions to follow in the days leading up to your appointment. The purpose of these preparations is to make sure your large intestine is as clean and clear as possible for your colonoscopy. If it isn’t, your endoscopist might not be able to see what they need to see. They might have to reschedule your colonoscopy, and you might have to redo these preparations another time.
Advertisement
You’ll begin by adjusting your diet a few days ahead of your colonoscopy. Typically, you’ll eat a low-fiber diet for two or three days, followed by a clear liquid diet on the last day. The afternoon or evening before your colonoscopy, you’ll take a laxative formula to purge your bowels (by pooping everything out). You’ll spend the next several hours in and out of the bathroom a lot. Make yourself comfortable, then get a good night’s sleep. Your colonoscopy will usually occur the following morning.
You’ll need to bring someone with you to your appointment who can drive you home. Since it takes a full day for the anesthesia to completely wear off, most healthcare places won’t check you in for your colonoscopy unless you have a responsible driver with you. (They’ll be hanging out for about two hours altogether.) After check-in, a healthcare provider will lead you to a room where you can change into a hospital gown. A nurse will install an IV line into your arm to begin delivering sedatives and pain medication to your bloodstream.
You can have general anesthesia (a controlled loss of consciousness, like sleeping) or you can have conscious sedation (a depression of awareness — you might fall asleep or stay awake, but in either case, you probably won’t remember it much afterward). You’ll discuss your options for anesthesia with a healthcare provider in advance, so you’ll know what to expect on the day of the procedure. Your healthcare provider will help you select the right type for your body and your needs.
Advertisement
With sedation, you shouldn’t feel pain inside your colon. This is true even if a provider removes tissue or performs laser therapy inside your colon. But you might feel a little gas pain or pressure when the colonoscope advances into your colon. That’s because the colonoscope actually blows carbon dioxide gas into your colon to inflate it for better viewing. It’s usually not too noticeable once the inflation part is done. You’ll be lying comfortably in the fetal position on a hospital bed, and you may even sleep.
A gastroenterologist or a colorectal surgeon performs most colonoscopies. Both are specialists in gastrointestinal diseases and receive special training in endoscopic procedures involving your gastrointestinal (GI) tract. Endoscopic procedures like colonoscopy aren’t just for looking inside your body — they can also be interactive. Endoscopists can take tissue samples and perform minor interventions through the endoscope. Their certification qualifies them to perform these procedures and to interpret the results.
Advertisement
It takes about 15 minutes to advance the colonoscope to the end of your large intestine and another 15 minutes to bring it back out the way it came. In this way, the doctor examines your entire large intestine twice. If they find something in the process that they need to remove or treat, this will add extra time. Colon polyps are common: they turn up in about 30% of routine colonoscopies. Although most are benign, it’s standard procedure to remove them on sight. This may add another 15 minutes.
You’ll spend the first hour after your procedure recovering in the healthcare center. This is so you have time to wake up from the anesthesia. Your healthcare team will continue to monitor your vital signs and watch for any signs of complications. When you’re awake, your gastroenterologist will go over what they found during the exam and any procedures they performed. You’ll also get a formal report by mail or electronically. If they took a tissue sample for biopsy, you’ll get those test results a little later.
It takes about 24 hours for the anesthesia to wear off completely. That’s why healthcare providers recommend you don’t drive, operate equipment or make important decisions until the next day. But you’ll feel more like yourself every hour. You might feel some gas pain, bloating or nausea in the first hour or two, but this should pass quickly. You can return to your normal diet as soon as you feel ready. If the provider removed the tissue, you might have some light rectal bleeding for a few days afterward.
Risks and complications are rare but possible. They include:
Most results you’ll know right away. Your provider will be able to tell you what they found, what procedures they performed and if they succeeded. If they removed tissue for biopsy, they won’t have those results for another few days to weeks. Removing tissue and sending it to a lab doesn’t always mean that your gastroenterologist suspects cancer. It could just be a precaution, or they could be looking for something else, like microscopic colitis. They’ll let you know what they expect to find.
Abnormal results may include:
Your doctor will discuss your results with you and what they mean.
Video content: This video is available to watch online.
View video online (https://cdnapisec.kaltura.com/p/2207941/sp/220794100/playManifest/entryId/1_q3u020ft/flavorId/1_5f3sgelj/format/url/protocol/https/a.mp4)
Learn why you should get a colonoscopy.
There are several other screening tests for colorectal cancer. Colonoscopy is the most sensitive test, meaning it’s the most likely to detect early cancer or precancerous conditions. Detecting potential cancer as early as possible is important to preventing and treating it effectively. Colonoscopy is also the only screening test for colorectal cancer that’s both diagnostic and therapeutic at the same time. When doctors find suspicious tissue during a colonoscopy, they can remove it during the same procedure.
Alternative screening tests for colon cancer include:
Advantages of a traditional colonoscopy include:
A colonoscopy can be diagnostic, therapeutic and preventive all at the same time. It may seem like a lot to go through if you don’t have a disease, but if you do, this makes an important difference. Colorectal cancer is the third-leading cause of cancer death in the United States. It’s preventable, but only when detected early. Colonoscopies allow healthcare providers to detect and treat cancer before it develops or spreads and before you have symptoms. If you’re clear, you’ll only need one every 10 years.

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
A colonoscopy or other screening is an important test for colon cancer. The team at Cleveland Clinic can give you peace of mind and expert care when you need it.
