Chronic pain lasts months or years and can affect any part of your body. It interferes with daily life and can lead to depression and anxiety. The first step in chronic pain management is to find and treat the cause. When that isn’t possible, the most effective approach is a combination of medications, therapies and lifestyle changes.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Chronic pain is pain that lasts for over three months. You may feel the pain all the time or it may come and go. It can happen anywhere in your body and has countless causes.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Chronic pain is a very common condition and one of the most common reasons why people seek medical care. In 2021, about 20.9% of U.S. adults (51.6 million people) experienced chronic pain, according to a study from the U.S. Centers for Disease Control and Prevention (CDC).
Pain is your body’s way of telling you that something’s wrong, like an alarm. But when that alarm continues to go off for months or years, it can drown out many aspects of life that bring you joy. And it can take quite a toll on your physical, mental and emotional health. Because of this, it’s essential to seek help for chronic pain. Together, you and your healthcare provider can develop a plan to help dampen chronic pain.
Chronic pain can come in many different forms and occur across your body. It’s the main symptom of a wide range of injuries, infections and diseases. Common types of chronic pain include:
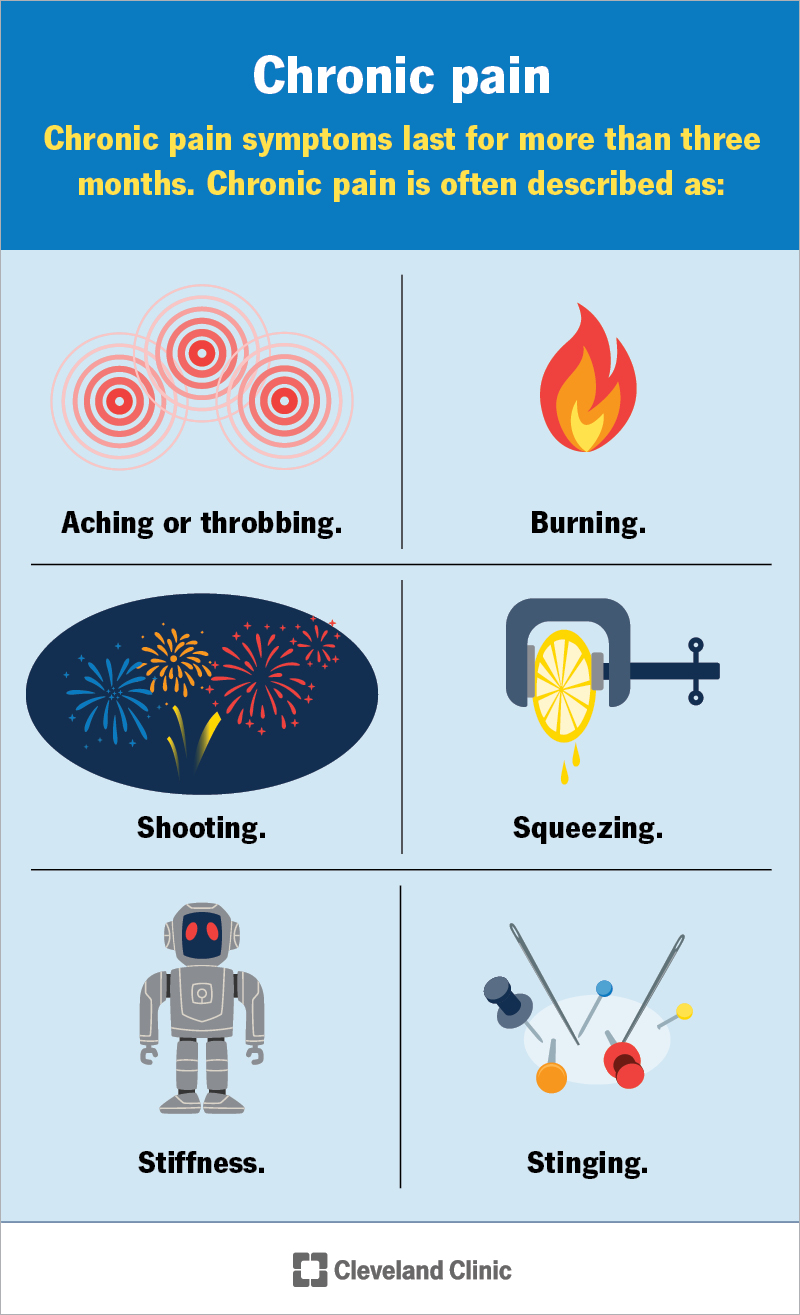
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/4798-chronic-pain)
Chronic pain symptoms vary from person to person. But the defining characteristic of chronic pain is that it lasts for more than three months. You may describe the pain as:
Advertisement
Chronic pain often leads to other symptoms and conditions, including:
It’s important to see a healthcare provider if pain is interfering with your daily life.
Chronic pain is often very complex. Sometimes, it has an obvious cause — you may have a long-lasting condition like cancer or arthritis that leads to pain. Other times, it’s more difficult to find the underlying cause — or there may be several factors contributing to pain.
General types, or causes, of pain include:
Some people also have chronic pain that’s not tied to a direct physical cause. This doesn’t mean that your pain isn’t real. Oftentimes, this type of pain (psychogenic pain) is related to changes in your nervous system and other understandable emotional and psychological factors.
It’s possible to have several causes of pain overlap. You could have fibromyalgia in addition to back pain from degenerative disk disease, for example.
As many conditions or injuries can cause chronic pain, there are several risk factors for it. In general, some risk factors include:
Advertisement
Healthcare providers consider pain to be chronic if it lasts or comes and goes (recurs) for more than three months. Pain is usually a symptom, so your provider needs to determine what’s causing your pain, if possible. Pain is also subjective — only the person experiencing it can identify and describe it — so it can be difficult for providers to find the cause.
If you have long-lasting pain, see a provider. They’ll want to know:
Your provider may do a physical exam and recommend tests to look for the cause of the pain, like:
Your healthcare provider may recommend one approach or a combination of several chronic pain management techniques. It may involve treating the underlying cause of chronic pain and/or managing pain as a symptom. Research shows that a combination of therapies results in a more significant reduction in pain than relying solely on single treatments.
Advertisement
How well a particular treatment works varies from person to person — even for the same cause of chronic pain. Providers typically start with minimally invasive or conservative pain management therapies before trying riskier ones. But there’s no single “right” approach for pain management for all people.
Approaches to chronic pain management include:
Depending on the cause of your pain and your unique characteristics, it may take time — and several different therapies — before you find the right approach that works for you. Your pain management plan is more likely to be effective if you work closely with your provider or team and adjust the plan as your needs change. It’s also important to discuss the benefits and possible risks and side effects of each treatment.
Advertisement
Currently, there’s no cure for chronic pain, other than to identify and treat its cause. For example, treating arthritis can sometimes stop joint pain.
Many people with chronic pain don’t know its cause and can’t find a cure. They use a combination of medications, therapies and lifestyle changes to lessen their pain.
Chronic pain usually doesn’t go away, but you can manage it with a combination of strategies that work for you. Current chronic pain treatments reduce a person’s pain score by about 30%. Treatments also have a significant impact on your quality of life and can lessen the stress associated with having a chronic pain condition.
Researchers continue to study pain disorders and treatments. Advances in neuroscience and a better understanding of the human body should lead to more effective treatments in the future.
Unmanaged or undermanaged chronic pain can impact your quality of life and your ability to function day to day. This can affect your ability to take care of yourself, work and maintain relationships. It can also worsen chronic conditions.
Living with chronic pain also increases your risk of:
It’s essential to seek medical care if you’re experiencing chronic pain or any of these complications. While it may take a while to find the right combination of therapies that work for you, it’s worth undertaking.
If you or a loved one are thinking about suicide, dial 988 on your phone to reach the Suicide and Crisis Lifeline. Someone is available to help you 24/7.
See your healthcare provider if:
If you have chronic pain, it may be helpful to ask your healthcare provider the following questions:
Living with chronic pain can be extremely challenging. It can affect nearly all aspects of your life, from working and socializing to taking care of yourself or others. It may feel more like existing with pain than living.
There’s no “one-size-fits-all” for chronic pain management. And it can take time to find a pain management plan that works for you. But getting the care you need — and deserve — is worth pursuing. Talk to your healthcare provider or a pain management specialist about treatment options that can get you closer to living the life you want.

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Comprehensive pain recovery treatment plans can help you manage your pain levels and symptoms more easily.
