Comorbidities are medical conditions that coexist alongside a primary diagnosis and affect your health, including your treatment and outlook. Common comorbidities among hospitalized people include hypertension, diabetes and chronic lung disease. Multimorbidity is a similar term that means one person has two or more chronic conditions.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Comorbidities are medical conditions that you have in addition to a primary diagnosis. You may have one or more comorbidities. Morbidity is a medical term that refers to the state of having a specific disease or condition. So, adding “co” in front of this word means two or more conditions occur together.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Comorbidity might feel like a scary word. But learning what it means and how it affects your health can help you take an active role in your care. This is because comorbidities can interact in ways that affect your approach to managing your health.
For instance, your healthcare provider might encourage you to increase your physical activity to manage obesity. But what if you soon learn that you have osteoarthritis? In that case, you might choose to replace daily walks with water aerobics to prevent flare-ups of joint pain. Osteoarthritis is an example of a comorbidity that might change your approach to managing obesity.
High blood pressure (hypertension) is another example of a comorbidity. People with other diagnoses like heart or lung diseases can also have high blood pressure. If you have high blood pressure alongside other conditions, your provider will be mindful of these coexisting conditions. This might involve prescribing blood pressure medication that won’t interact with any of your other medications.
The concept of comorbidities is very important in healthcare. So, learning about what it means can help you have conversations with your provider and better understand your care plan. This knowledge can also help you support loved ones through their diagnoses.
Advertisement
Other terms that people use to describe comorbidities include:
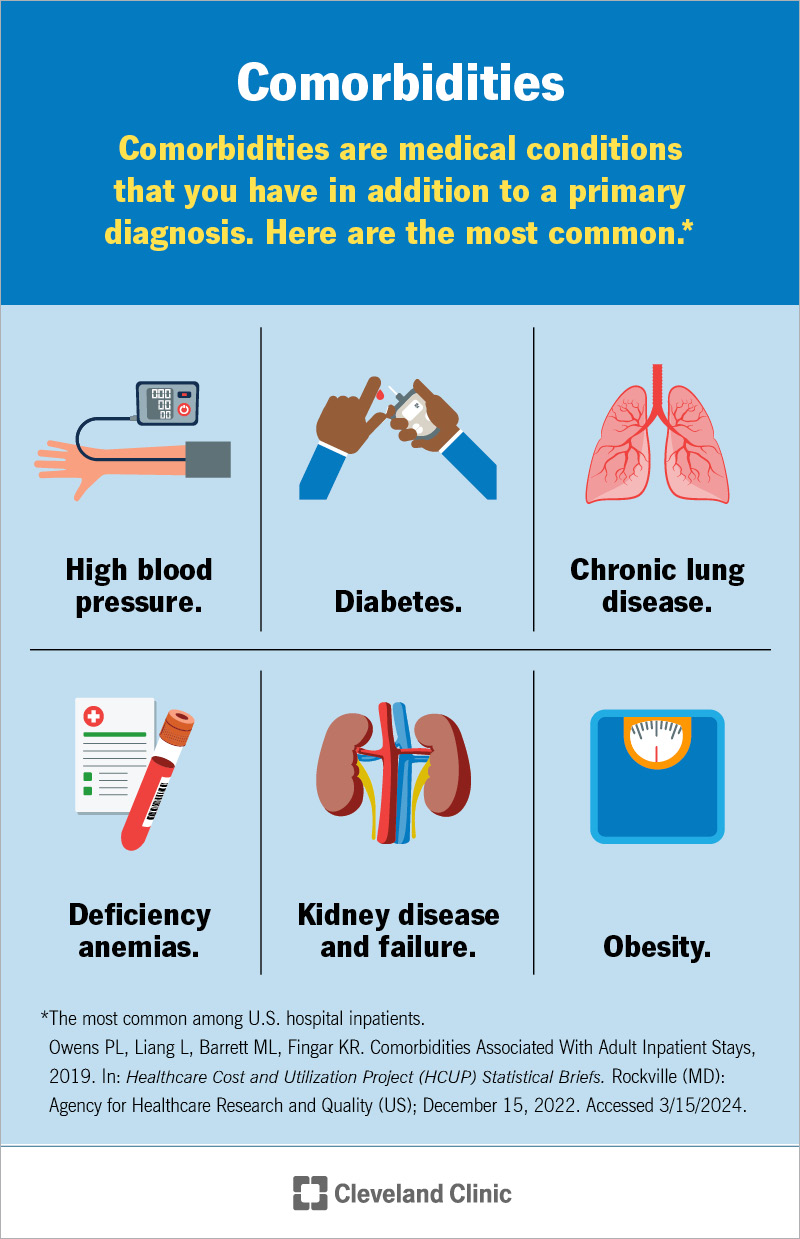
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/comorbidities.jpg)
Hospitalized people typically have at least one comorbidity, including common conditions like high blood pressure and diabetes.
Comorbidity is a distinct medical diagnosis that you have alongside one primary diagnosis (sometimes called a principal diagnosis or index disease). You might wonder, what’s a primary diagnosis? This is where defining terms gets a bit tricky.
In the medical world, a primary diagnosis is the condition you’re receiving care for at a certain moment or within a specific timeframe. It may be the condition that’s most serious or most in need of specialized care. Or it might be the condition that sends you to the hospital.
A specific healthcare provider designates a condition as primary. Your primary condition can change according to which healthcare provider you’re seeing and how your health evolves.
For example, let’s say you have chronic kidney disease, high blood pressure and Type 2 diabetes. You regularly see your nephrologist (kidney specialist), who treats your kidney disease. Your nephrologist will view kidney disease as your primary diagnosis because this is the focus of the care they provide. They’ll view high blood pressure and diabetes as comorbidities of kidney disease. Your nephrologist takes these comorbidities into account when treating your kidney disease.
To continue with this example, let’s say you also regularly see your endocrinologist, who helps you manage diabetes. This provider will view diabetes as your primary diagnosis. They’ll see your kidney disease and high blood pressure as the comorbid conditions.
What a primary diagnosis is and what a comorbidity is can therefore shift depending on the situation. Specialists often see your health in terms of a main diagnosis and its comorbidities. But your primary care provider or others might view things slightly differently. They may use the concept of multimorbidity to capture a broader view of your health.
When you think of your health in terms of comorbidities, one diagnosis is central. If you drew this out on a chalkboard, there would be one big circle in the middle with lines extending outward in all directions. Each line would connect to another circle. Your primary diagnosis would go in the central circle, and a comorbidity would go in each of the surrounding circles. You can see all the circles at once, but chances are, your eyes keep returning to that central circle. All the radiating lines draw your attention back to it. It’s your main focus at this moment.
When your provider views your health in terms of comorbidities, they recognize that one diagnosis needs to take center stage for a while. They’ll talk to you about why that’s the case and how managing that condition might affect any comorbidities. They’ll also tell you how any comorbidities affect their approach to managing your primary diagnosis.
Advertisement
The U.S. Department of Health and Human Services defines multimorbidity as having at least two medical diseases or conditions that each last more than one year. This definition doesn’t mention a primary diagnosis, which makes it different from the definition of comorbidities.
Many researchers use the concept of multimorbidity to explore how diagnoses interact. Still, people often use comorbidities and multimorbidity to mean the same thing: the state of having two or more medical conditions.
Having comorbidities or multimorbidity can affect your health in many ways. When you have two or more chronic conditions:
Advertisement
Many different comorbidities affect people staying in hospitals (inpatients) as well as people diagnosed with various medical conditions.
One study looked at comorbidities among adult inpatients in U.S. hospitals in 2019. That year, over 84% of all hospital stays involved people who had one or more comorbidities. These comorbidities were separate from their principal diagnosis (the reason for their hospitalization). Of this group, about 50% had at least three comorbidities.
This study found the most common comorbidities were:
This study also found:
Advertisement
Researchers often study people with one specific condition — like arthritis or heart failure — to see what additional conditions (comorbidities) those people are living with. Of course, each person is different, and this research doesn’t suggest that everyone with a specific diagnosis will necessarily have certain comorbidities. But it does shed light on common patterns that have emerged.
Attention-deficit/hyperactivity disorder (ADHD)
Common comorbidities include:
Arthritis
Common comorbidities include:
Chronic obstructive pulmonary disease (COPD)
Common comorbidities include:
Heart failure
Common comorbidities include:
Type 2 diabetes
Common comorbidities include:
Sometimes, conditions occur together because they share common causes or risk factors. For example, both high blood pressure and diabetes can lead to an increased risk of heart disease and kidney disease. But other times, comorbidities don’t share an underlying cause. Your healthcare provider can tell you more about the possible causes of any diagnoses you have and how treatment can help.
Learning the meaning of comorbidities and multimorbidity can help you talk to your healthcare provider about your health. But when you feel yourself getting too caught up in the vocabulary, take a step back.
What’s most important isn’t mastering all the medical terminology. It’s taking the time to learn about your diagnoses and how they affect your health. It’s understanding what treatments you might need, why you need them and how to manage medications at home. It’s knowing that no two people experience the same condition or combination of conditions in the same way.
Take all your questions and concerns to your provider so they can give you guidance tailored to your unique situation.

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s primary care providers offer lifelong medical care. From sinus infections and high blood pressure to preventive screening, we’re here for you.
