Overview
The Cleveland Clinic Children's Pediatric Liver Transplant Program provides special care for children who suffer from various types of liver disease that require liver transplantation. Our multidisciplinary team stays with your child and your family from the time of referral to transplant, and more importantly all the way through long-term care after transplant if a transplant is required.
While many of the causes leading to the need for a liver transplant may not be the same, they still need intense, collaborative support by multispecialty caregivers. Our program consists of five hepatologists with Certificates of Added Qualifications in Pediatric Transplant Hepatology from the American Board of Pediatrics who deal with all forms of liver disease, whether it requires surgery or transplant or not. Our transplant surgeons, when needed, have years of experience in taking care of children and infants. When an infant or child needs a liver transplant, you can be comforted knowing we have one of the most experienced teams in the country. We have a dedicated team of dietitians to help with common nutritional problems, like malnutrition and vitamin deficiencies, in patients with liver disease. Because liver problems are often chronic, they may affect the way the child or family copes with their problems. These problems can be very stressful and we actively involve our transplant-dedicated psychologists to help. In addition, we have social workers and pediatric transplant pharmacists to help as well.
Because liver transplant is a lifetime commitment, the Cleveland Clinic Children's Pediatric Liver Transplant Program makes it our priority to make sure your child receives the best treatment and to support your child and your family along your individual transplant journey.
What We Treat
Our pediatric liver disease program treats infants and children covering the whole spectrum of pediatric liver disease. Once they age into young adults, we are able to maintain continuity of care by transitioning them to caregivers in collaboration with our adult liver transplant program. Whether your child’s illness can be managed with medications or surgery, we as a team will give them the best of care regardless of their needs.
Diseases we treat
- Metabolic liver disease (such as urea cycle defects, glycogen storage diseases, Wilson's disease, or mitochondrial disorders)
- Viral hepatitis (e.g. hepatitis B or C, EBV hepatitis)
- Acute liver failure
- Chronic liver disease & chronic jaundice
- Autoimmune liver disease, including primary sclerosing cholangitis (PSC)
- Non-alcoholic fatty liver disease (NAFLD) and non-alcoholic steatohepatitis (NASH)
- Progressive familial intrahepatic cholestasis (PFIC), including Byler's disease
- Biliary atresia
- Alagille syndrome
- Alpha-1 antitrypsin deficiency
- Cirrhosis
- Cystic fibrosis associated liver disease
- Drug toxicity
- Abnormal or elevated liver enzymes
- Liver tumors, including hepatoblastoma and hepatocellular Carcinoma
- Liver cancer
- Liver transplant
- Neonatal jaundice and/or neonatal cholestasis
There are a variety of reasons for why a child may need a liver transplant. Liver transplantation is required when the liver is irreversibly damaged to the point where the liver can not sustain a child’s life or their liver disease is seriously compromising their quality of life (e.g. intractable pruritus).
In advanced liver disease, some or all of the following signs may appear:
- Jaundice (yellow coloring of the skin and eyes)
- Itching (also known as pruritus)
- Nausea, vomiting, and/or loss of appetite
- Poor weight gain
- Tendency to bruise and bleed easily
- Ascites (fluid in the abdomen)
- Swelling in the legs and feet due to fluid accumulation
- Fatigue and decreased energy
- Clay-colored stools
- Dark, tea-colored urine
- Mental confusion, possibly progressing to coma
- Vomiting blood or passing blood in the stool
Irreversible liver failure isn’t the only reason that one may need a liver transplant. Children can become ill when the liver makes an abnormal protein or does not make an important protein (for example, in metabolic disorders). In metabolic disorders, liver function tests are generally normal, but medical conditions caused by some metabolic disorders can seriously affect a child's quality of life and can even be fatal. Liver transplant offers the only chance for some of these children to become healthy and live longer.
What to Expect

When you visit the Cleveland Clinic Children's Pediatric Liver Transplant Program for the first time, we assess the status of your child’s general condition and the impact of their liver disease. After thorough evaluation by our multidisciplinary team, we provide you with all treatment options, and not just limited to the potential need for a liver transplantation.
During your evaluation, you and your child will meet with the following experts:
- Pediatric transplant hepatologist.
- Liver transplant surgeon.
- Pediatric anesthesiologist.
- Pediatric liver transplant nurse practitioner.
- Transplant pharmacist.
- Dietitian focused on liver disease.
- Transplant social worker.
- Financial counselor.
Types of Liver Transplant
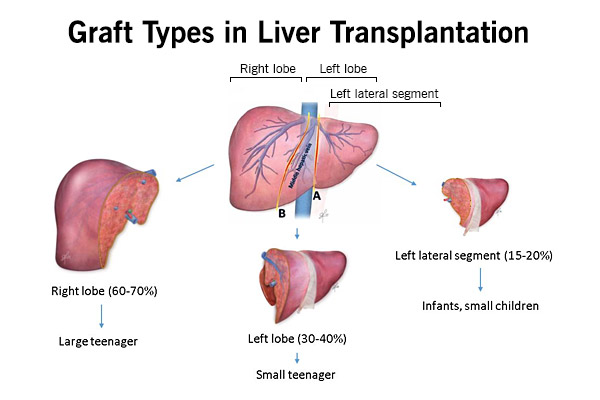
Finding a size-matched donor liver is very important in achieving good outcomes in pediatric liver transplantation. However, it is not easy to find a size-matched deceased donor for children who are waiting for liver transplantation. To maximize the opportunity for your child to receive a liver transplant before becoming too ill, we often use partial livers (technically modified liver graft). Based on what your child needs, we can provide the following types of liver transplantation:
- Living donor liver transplantation: A portion of the liver is donated by a healthy adult (age 18-60 years). Our center also has a well-established anonymous living donor liver transplantation program, wherein charitable non-related donors can donate a portion of their liver to those in need.
- Split liver transplantation: A liver from a deceased donor is split into two portions to save 2 patients at the same time
- Reduced-size liver transplantation: Size of the liver from a deceased donor is surgically reduced to transplant a small child
- Whole liver transplantation: A liver from a size-matched deceased donor is used without surgical modification on the donor liver
When your child needs a liver transplant, it is very important to provide this treatment before your child becomes too ill to have a liver transplant. This is the main reason that we offer several options to using partial livers for a patient's liver transplant procedure.
Appointments
Learn more about pediatric hepatology or pediatric liver transplantation at Cleveland Clinic Children's, or to schedule a consultation with one of our providers, please contact:
Kristin Burns, Cleveland Clinic Children’s
Phone: 216.444.9322
Email: burnsk8@ccf.org



