An arrhythmia is a heart rhythm that isn’t normal. Your heart may be beating too fast when you’re at rest or just not beating in a regular pattern, for example. Arrhythmias range from harmless to serious, with symptoms and without. There are many options to treat arrhythmias, but some don’t need them. The prognosis varies greatly depending on the type.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
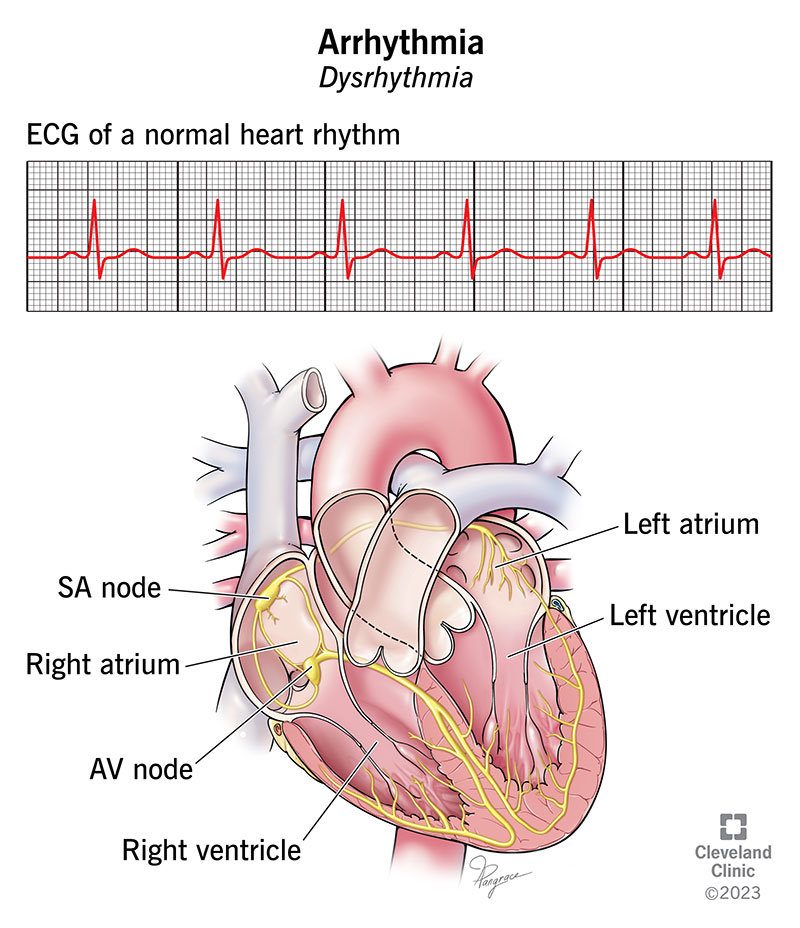
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/16749-arrhythmia-illustration)
An arrhythmia (also called dysrhythmia) is an abnormal heartbeat. Arrhythmias can start in different parts of your heart and they can be too fast, too slow or just irregular.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Normally, your heart beats in an organized, coordinated way. Issues with various parts of your heart — or even the blood your heart pumps — can affect your heart’s normal rhythm. Having a normal heart rhythm matters because your heart supplies your whole body with nutrients and oxygen through the blood it pumps.
Some types of arrhythmia are harmless and don’t require treatment. Others can put you at risk for cardiac arrest. Many are in between these two extremes. A healthcare provider can tell you which type of arrhythmia you have and what kind of treatment you need, if any.
Healthcare providers describe arrhythmias by where in your heart they start.
An estimated 1.5% to 5% of people have arrhythmias. However, some people don’t have symptoms, making it difficult to estimate how many people actually have arrhythmias. In the U.S., atrial fibrillation is the most common type of arrhythmia.
Advertisement
Heart arrhythmia symptoms may include:
A cardiac arrhythmia may be “silent” and not cause any symptoms.
Arrhythmia causes include:
Most arrhythmias happen because of an issue with your heart’s arteries, valves or muscles.
Risk factors for arrhythmia include:
Without treatment, arrhythmias can lead to complications such as:
A healthcare provider can find an irregular heartbeat during an examination by taking your pulse and listening to your heart.
After assessing your symptoms and performing a physical examination, they may order diagnostic tests to help confirm that you have an arrhythmia. This can also help find the cause.
You may also want to see an electrophysiologist — a cardiologist who has additional specialized training in the diagnosis and treatment of heart rhythm disorders.
Some tests that can check for an irregular heart rhythm and associated diseases include:
Treatment depends on the type and severity of your arrhythmia. In some cases, no treatment is necessary. Heart arrhythmia treatment options include:
Many medications can treat arrhythmias. Because everyone is different, you may have to try several medications and doses to find the one that works best for you. Heart arrhythmia treatments include:
Advertisement
It’s important to know:
Simple changes to the way you live can help with arrhythmias. These changes may include:
In addition to medicine, some people need therapies to treat or eliminate irregular heart rhythms. Your healthcare provider will determine the best treatment for you and discuss the benefits and risks of these therapies with you.
Therapies include:
Advertisement
A cardiologist may insert certain devices during a procedure in the electrophysiology lab. Devices to treat a heart arrhythmia include:
People with arrhythmias may require heart surgery for any of these reasons:
Advertisement
Side effects and complications vary depending on the treatment. They may include:
Arrhythmia medication
Cardioversion
Catheter ablation
Pulmonary vein isolation
Devices
Surgery
It may take a little time to find the right medication and dose that works for your arrhythmia. Depending on the procedure or surgery, recovery afterward can take weeks or months. If you have a procedure like catheter ablation or pulmonary vein isolation, you may still have arrhythmias for several weeks while you’re healing. Your provider can tell you what to expect in your specific situation.
Depending on the type of cardiac arrhythmia you have, you may have mild or severe symptoms or none at all. You may not need treatment, but some people need medicine or a procedure. With heart arrhythmia treatment, many people can live full lives. Some people with more serious arrhythmias have a cardiac arrest and may or may not survive.
Harmless arrhythmias go away and come back in response to what triggers them. However, people with other types of arrhythmias — especially those that put you at risk for cardiac arrest — need treatment for the rest of their lives.
Here are some ways to lower your risk of arrhythmia:
If you have a cardiac arrhythmia, you might find it useful to know how to take your pulse. Your pulse is your heart rate, or the number of times your heart beats in 1 minute. Pulse rates vary from person to person. Your pulse is slower when you’re at rest and increases when you exercise. A normal heart rate (at rest) is 60 to 100 beats per minute. If you have a fitness tracker or smartwatch, it can track your heart rate.
You should also make sure that your family and friends know how to recognize your arrhythmia symptoms. It can give you peace of mind if they learn how to start CPR.
If you have an arrhythmia, you should limit the amount of alcohol and caffeine you consume. Both of these can trigger arrhythmias.
Your provider will tell you how often you should visit. Call them in between visits if your symptoms become more frequent or severe.
You’ll need to visit your provider for regular follow-up visits to:
Get immediate medical care if you have:
Questions you may want to ask your provider include:
There are many ways for your heartbeat to be irregular. Some of these irregular heartbeats, called arrhythmias, don’t cause symptoms. It’s important to see your healthcare provider if you do notice symptoms like extreme fatigue or heart palpitations. Your provider will help determine the best treatment option for you, but you can also help yourself by making appropriate lifestyle changes.
Learn more about the Health Library and our editorial process.
Cleveland Clinic's health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability, and up-to-date clinical standards.
Cleveland Clinic's health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability, and up-to-date clinical standards.
When your heart rhythm is out of sync, the experts at Cleveland Clinic can find out why. We offer personalized care for all types of arrhythmias.
