Hypoglycemia (low blood sugar) is common in people who have diabetes. But it can also sometimes affect people without diabetes. You need to treat hypoglycemia as soon as possible by consuming carbohydrates. If it’s left untreated, severe low blood sugar can be life-threatening.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Hypoglycemia happens when the level of sugar (glucose) in your blood drops below the range that’s healthy for you. It’s also called low blood sugar or low blood glucose. Hypoglycemia is common in people with diabetes, especially Type 1 diabetes.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
For most people with diabetes, hypoglycemia is when your blood sugar level is below 70 milligrams per deciliter (mg/dL) or 3.9 millimoles per liter (mmol/L).
For most people without diabetes, hypoglycemia is when your blood sugar level is below 55 mg/dL or 3.1 mmol/L.
Hypoglycemia requires immediate treatment by eating or drinking sugar/carbohydrates. Severe hypoglycemia can be life-threatening and requires treatment with emergency glucagon and/or medical intervention.
Glucose (sugar) mainly comes from carbohydrates in the food and drinks you consume. It’s your body’s main source of energy. Your blood carries glucose to all of your body’s cells to use for energy. Glucose is very important because it’s the primary source of energy for your brain.
If you don’t have diabetes, several bodily processes naturally help keep your blood glucose in a healthy range. Insulin, a hormone your pancreas makes, is the most significant contributor to maintaining healthy blood sugar. Glucagon is another important hormone in this process.
People who have diabetes must use medication, like oral diabetes medications or synthetic insulin, and/or lifestyle changes to help keep their blood sugar levels in range.
Advertisement
Low blood sugar often happens due to excess insulin — whether your body naturally makes too much or you inject too much synthetic insulin. Other hormonal and metabolic issues can also lead to low blood sugar.
If your blood sugar drops below the healthy range, it causes certain symptoms like shakiness and a faster heartbeat and can be life-threatening if it goes too low. This is because your brain needs a continuous supply of glucose to function properly. Without enough glucose, your brain can’t function.
Hypoglycemia is common in people with diabetes, especially people who take insulin to manage the condition.
One study found that 4 in 5 people with Type 1 diabetes and nearly half of all people with Type 2 diabetes who take insulin reported a low blood sugar episode at least once over a four-week period.
People with Type 2 diabetes who take meglitinide or sulfonylurea oral diabetes medications are also at an increased risk for low blood sugar.
You can experience hypoglycemia without having diabetes, but it’s uncommon.
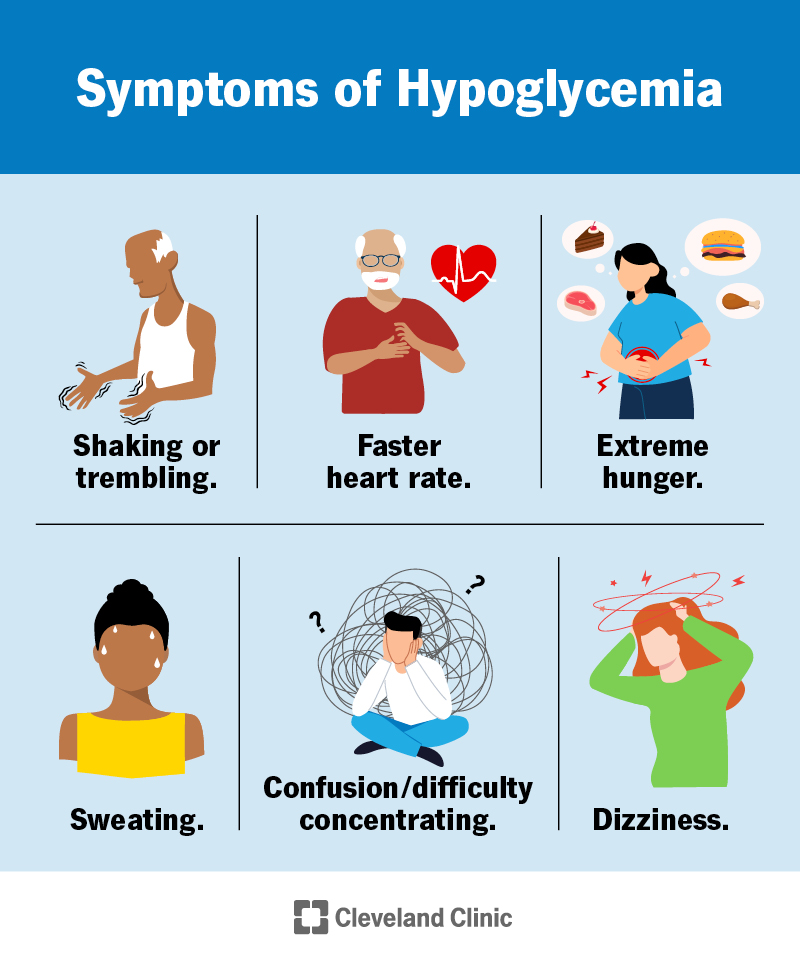
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/11647-hypoglycemia-low-blood-sugar)
Symptoms of hypoglycemia can start quickly, and they can vary from person to person. One person can also experience different symptoms for each episode.
The signs of hypoglycemia are unpleasant. But they provide good warnings that you should take action before your blood sugar drops more. The signs include:
Signs of severe hypoglycemia include:
Severe hypoglycemia is life-threatening. It needs immediate medical treatment. In rare cases, severe hypoglycemia that isn’t treated can result in a coma and/or death.
You can also experience low blood sugar while sleeping (nocturnal hypoglycemia). Symptoms may include:
The glucose level at which symptoms begin varies from person to person for people who have diabetes.
In general, symptoms often begin for people with diabetes when their blood glucose is around 70 mg/dL or lower. If your blood sugar is falling rapidly, you may experience symptoms before this point.
Some people with diabetes can have symptoms of hypoglycemia at relatively higher glucose levels. This is because, when you have chronic hyperglycemia (high blood sugar), your body gets used to that as its “normal” level. It alters the set point at which low blood sugar symptoms become apparent.
Advertisement
Some people who have low blood sugar episodes don’t have symptoms or don’t notice them. Healthcare providers call this hypoglycemia unawareness. People with hypoglycemia unawareness are more likely to have severe episodes and need medical help.
Hypoglycemia unawareness can happen in people with diabetes who live with chronically low blood sugar levels. Their body stops having symptoms when low blood sugar occurs.
If you have hypoglycemia unawareness, it’s important to let your friends and family know so that they know how to help you if you experience a severe low blood sugar episode. You may also benefit from the following:
Prolonged severe hypoglycemia is life-threatening and can lead to the following complications:
Operating heavy equipment, such as driving a vehicle, while having low blood sugar can also be dangerous. You may be more likely to get in an accident. If you have diabetes, always make sure your blood sugar is in range before operating heavy equipment.
Advertisement
Hypoglycemia happens when your blood sugar drops below a healthy range. Several factors can contribute to this for people with diabetes. Hypoglycemia can develop if things like food, exercise and diabetes medications are out of balance.
Common situations that can lead to hypoglycemia for people with diabetes include:
If you’re pregnant and have Type 1 diabetes, you’re also more likely to experience low blood sugar during the first trimester due to hormone changes.
There are two main types of non-diabetes-related hypoglycemia: reactive hypoglycemia and fasting hypoglycemia.
Reactive hypoglycemia happens when you experience low blood sugar after a meal. It typically occurs about two to four hours after a meal.
Researchers don’t yet know the exact cause. But they think it happens due to a sudden spike and then fall in blood sugar after eating certain foods, especially simple carbohydrate foods like white rice, potatoes, white bread, cake and pastries.
Advertisement
Bariatric surgery can also result in reactive hypoglycemia. After certain types of bariatric surgery, such as gastric bypass surgery, your body absorbs sugars very quickly, which stimulates excess insulin production. This can then cause hypoglycemia.
Your body usually corrects reactive hypoglycemia on its own, but consuming carbohydrates may help your symptoms go away more quickly.
For the majority of people without diabetes, not eating food for a long time (fasting) doesn’t lead to hypoglycemia. This is because your body uses hormones and stored glucose to manage your blood sugar.
However, certain conditions and situations can lead to fasting hypoglycemia in people without diabetes, including:
In rare cases, non-diabetes-related medications can lead to hypoglycemia, such as beta-blockers and certain antibiotics.
If you’re experiencing hypoglycemia and don’t have diabetes, talk to your healthcare provider.
The only way to know if you have hypoglycemia is to check your blood sugar with a blood glucose meter (glucometer). Most of these devices use a tiny blood sample from a finger prick with a lancet (small needle).
A CGM could be a helpful tool in identifying and preventing low blood sugar because you can program it to alert you to low blood sugar. CGM alerts can be especially useful during times when it could be dangerous to have a low blood sugar, such as while you’re sleeping or driving.
If you’re experiencing symptoms of hypoglycemia and are unable to check your blood sugar, treat the hypoglycemia.
If your healthcare provider suspects you have hypoglycemia, they may check your blood sugar every few hours during a fast lasting several days. You’ll need additional tests to determine the underlying cause of the hypoglycemia, such as imaging tests to see if a tumor is causing the low blood sugar episodes.
For reactive hypoglycemia, your provider might recommend a test called a mixed-meal tolerance test (MMTT). For the MMTT, you first have a special drink containing protein, fats and sugar. The drink raises your blood glucose, causing your body to make more insulin. Then a provider will check your blood glucose multiple times over the next five hours.
You treat mild to moderate hypoglycemia by eating or drinking sugar (carbohydrates).
The American Diabetes Association recommends the “15-15 rule” to treat an episode of mild to moderate hypoglycemia:
To know how many carbs you’re eating, read food nutrition labels. Some examples of foods that contain about 15 grams of fast-acting carbs include:
If you have symptoms of hypoglycemia but can’t check your blood sugar, use the 15-15 rule until you feel better.
Children may need fewer grams of carbs to treat hypoglycemia. Check with your child’s healthcare provider.
Severe hypoglycemia requires different treatment than mild or moderate hypoglycemia. If someone you know is having a hypoglycemia episode and is slurring their speech, disoriented or unconscious, don’t give them food or liquid. They could choke.
Severe hypoglycemia episodes require the use of emergency glucagon. This is a synthetic form of glucagon that you can administer as an injection or nasal powder (dry nasal spray), depending on the type. Synthetic glucagon triggers your liver to release stored glucose, which then raises blood sugar.
If the glucagon is injectable, inject it into their butt, arm or thigh, following the instructions in the kit. If the glucagon is a nasal powder, follow the instructions on the package to administer it into their nostril.
When the person regains consciousness (usually in 5 to 15 minutes), they may experience nausea and vomiting. If they’re lying down, roll them onto their side to prevent choking in case they vomit.
Don’t hesitate to call 911 for help. If someone is unconscious and glucagon isn’t available or you don’t know how to use it, call 911 immediately.
The prognosis (outlook) of non-diabetes-related hypoglycemia varies depending on the underlying cause.
Having frequent hypoglycemia episodes can be dangerous if you have diabetes. It can lead to hypoglycemia unawareness, which means you don’t experience warning signs of low blood sugar. It’s important to see a healthcare provider who helps you manage diabetes if you’re having frequent lows.
Unfortunately, it can be difficult to totally prevent low blood sugar when you have diabetes. But you can adjust your diabetes management plan to try to lower the number of hypoglycemia episodes you experience.
It’s easiest to do this when you and your healthcare provider understand what causes your blood sugar to drop. Give your healthcare provider as much information as possible about any low blood sugar episodes. Fixing the problem may be as simple as changing the times you take medication, eating and exercise.
The following steps can help prevent low blood sugar:
If you have diabetes or another condition that causes hypoglycemia, wear a medical alert necklace or bracelet or carry a medical ID. That way, people know how to help you in case of an emergency.
Steps you can take to prevent severe hypoglycemia include:
If you have diabetes, try not to over-treat low blood sugar by eating an excess amount of carbs. This can lead to rebound high blood sugar. It can be difficult to not overeat due to your body’s “fight or flight” response. Once you’ve initially treated the low with 15 grams of carbs, set a timer for 15 minutes before consuming more sugar.
If you have diabetes and are experiencing frequent low blood sugar episodes, talk to a provider who helps you manage diabetes. They can help you adjust your management plan, which may include changes to your medication regimen, meal plans or exercise routine.
If you don’t have diabetes and are experiencing low blood sugar, talk to your healthcare provider. They’ll need to order tests to determine the underlying cause. In some cases, the underlying condition can be serious. Because of this, it’s important to see your provider.
Hypoglycemia is low blood sugar. “Hypo-” means “below.” Hyperglycemia is high blood sugar. “Hyper-” means “above” or “beyond.”
Hypoglycemia is quite common in people with diabetes. If it’s not treated in time, it can be life-threatening. It’s important to learn your personal warning signs for low blood sugar and to monitor your blood sugar regularly to try to prevent severe low blood sugar. Work with your healthcare provider to adjust your diabetes management plan if you’re experiencing frequent hypoglycemia. The more you know about what’s causing the episodes, the easier it’ll be to adjust your plan.
If you’re experiencing low blood sugar and don’t have diabetes, you should see your healthcare provider. While it’s rare that the underlying cause is a serious condition, it’s possible. It’s better to get checked out sooner rather than later.

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s primary care providers offer lifelong medical care. From sinus infections and high blood pressure to preventive screening, we’re here for you.
