Insulinoma is a rare tumor that releases excess insulin. This causes low blood sugar episodes. Most cases of insulinoma don’t spread to other areas of your body. And most cases are curable with surgery.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
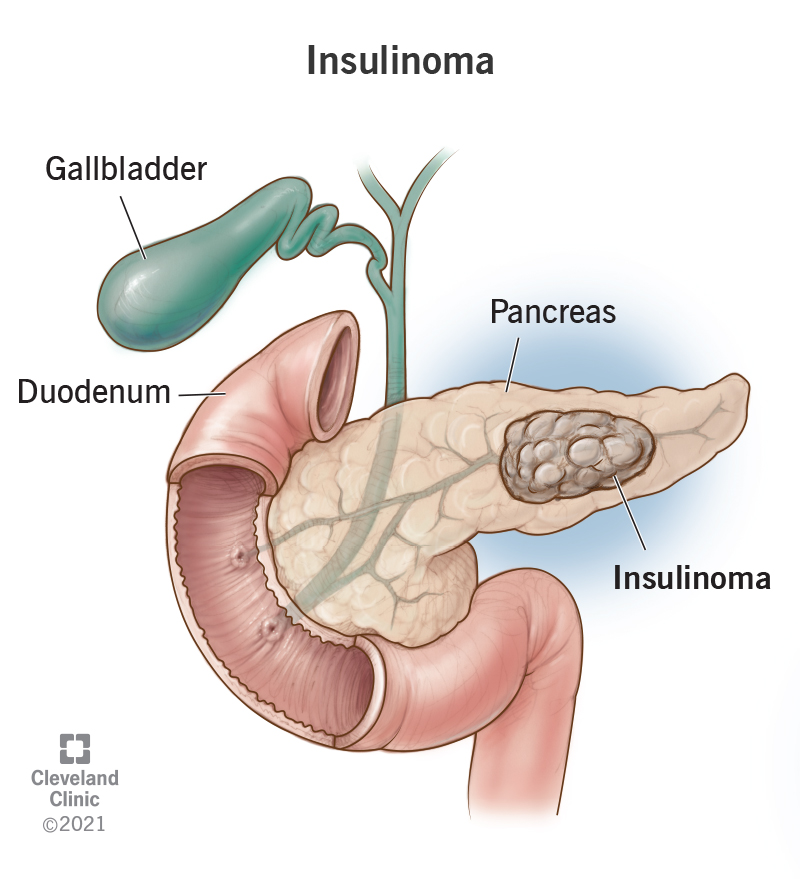
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/22217-insulinoma)
Insulinoma is a rare tumor in your pancreas that releases excess insulin. Insulin is the hormone that helps keep your blood sugar (glucose) at healthy levels.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Insulinoma is one of several pancreatic neuroendocrine tumors (pNETs). These are rare tumors that start in your pancreas’s endocrine cells.
About 85% to 90% of insulinomas are nonmetastatic (“indolent”). This means they don’t spread outside of your pancreas (metastasize). Metastatic (“aggressive”) insulinomas are very rare. Metastatic insulinomas are most likely to spread to your lymph nodes and/or liver.
Insulinomas release insulin. If you have insulinoma, it typically floods your body with insulin. This results in low blood sugar (hypoglycemia). When that happens, you may feel shaky. You may also feel like your heart is racing. In extreme circumstances, you may faint or have seizures.
Your symptoms should improve if you consume something that has sugar (carbohydrates). This could include apple juice, regular soda or a banana.
Experiencing low blood sugar can be scary, especially when you don’t know why it’s happening or when it’ll strike again. Keep snacks on hand and see your healthcare provider as soon as possible.
Insulinomas mainly cause low blood sugar (hypoglycemia) episodes. Symptoms of low blood sugar include:
Advertisement
Symptoms of severe low blood sugar include:
Most people with insulinoma experience low blood sugar when fasting — usually in the morning when they wake up. Some people with insulinoma experience low blood sugar episodes after meals.
Persistent hypoglycemia can interfere with daily activities and cause irreversible brain damage. It can even lead to coma and death. It’s very important to see your healthcare provider if you have low blood sugar symptoms.
Insulinomas happen when the cells in your pancreas that create insulin multiply uncontrollably. Researchers aren’t sure why that happens.
But they do know that insulinoma can happen alongside multiple endocrine neoplasia type 1 (MEN1). This is an inherited condition in which multiple tumors affect different parts of your endocrine system. About 5% to 10% of insulinoma cases affect people with MEN1.
If one of your first-degree relatives (biological parents and siblings) has a MEN1 diagnosis, talk to your healthcare provider. They can recommend genetic testing that can screen for the condition. If you have MEN1, genetic testing could help detect tumors in their early phases.
Your healthcare provider will likely suspect you have insulinoma if you have the following signs (called Whipple’s triad):
They’ll then recommend some tests to help diagnose insulinoma.
Your provider may recommend fasting up to 72 hours to bring on a low blood sugar episode. This is the gold-standard test for diagnosing insulinoma. But you won’t be alone. A provider will monitor you during your fast.
Once you develop low blood sugar symptoms, you’ll get blood tests that check your:
After the blood draw, a provider will give you treatment for the low blood sugar.
The results of these tests can show if too much insulin (hyperinsulinemia) is causing your low blood sugar episodes.
If the 72-hour fast points to insulinoma, your provider may suggest one or more of the following imaging tests:
These tests can assess the tumor’s size and its location in your pancreas. If imaging tests don’t provide enough information, your provider may recommend a selective arterial calcium stimulation test. For this test, a provider measures insulin levels in your hepatic (liver) vein after stimulating arteries in various parts of your pancreas.
Advertisement
Surgery is the main treatment for nonmetastatic (indolent) insulinomas. Surgical options include:
Each of these surgeries has different risks. Your provider will go over the risks and which surgery would be best for you.
In the time leading up to surgery (or if surgery isn’t possible), it’s important to prevent and treat low blood sugar episodes. Your provider may recommend getting a continuous glucose monitoring (CGM) system. A CGM can help you catch low blood sugar episodes before they get too severe, especially during the night.
It’s important to remember that you shouldn’t use a CGM to diagnose insulinoma or other low blood sugar conditions. They’re for monitoring conditions after a diagnosis.
Your provider may recommend one or more of the following treatments for low blood sugar:
Advertisement
It’s important to wear medical identification that states that you experience low blood sugar. This way, someone can get you help as soon as possible if you have a severe episode. Also, tell people close to you about your low blood sugar episodes and how they can help.
Your provider may recommend combining surgery with other treatments for metastatic (aggressive) insulinoma. Or they may use medical treatments when surgery isn’t an option. Your provider might recommend:
Yes, most insulinomas can be cured with surgery. One study showed that 87% of people who had surgery for nonmetastatic insulinoma were alive 10 years after diagnosis. Your healthcare provider will consider factors like the tumor’s size and location before recommending a specific surgery.
Advertisement
The 10-year survival rate for metastatic insulinomas was 33%. It’s important to remember this is just an estimate. Your healthcare team will be able to give you a better idea of what to expect based on your unique situation.
Receiving a tumor diagnosis can be alarming and confusing, especially when it’s a rare one like insulinoma. The good news is that most insulinomas are curable with surgery. Even so, it’s not easy to learn you have a rare condition that requires surgery. Know that your healthcare team will be by your side to answer questions and support you. If you’re feeling like you’re mentally and emotionally on your own with insulinoma, ask your provider about services that might help.
Learn more about the Health Library and our editorial process.
Cleveland Clinic's health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability, and up-to-date clinical standards.
Cleveland Clinic's health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability, and up-to-date clinical standards.
A pancreatic cancer diagnosis can make your world tilt. Cleveland Clinic experts are here to start personalized treatment for the best possible outcome.
