If you’ve recently recovered from a stomach bug, UTI or STI and suddenly develop joint pain, you might have reactive arthritis. It's a rare type of autoimmune response to a bacterial infection somewhere in your body. Your immune system reacts with inflammation in your joints, eyes, skin or other tissues. Symptoms typically last for several months.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Reactive arthritis (Reiter’s syndrome) is a rare, temporary form of inflammatory arthritis that’s triggered by a bacterial infection. It causes pain and stiffness in your joints, especially in your lower body. It can also cause symptoms in other body tissues, like your eyes and skin, as well as whole-body symptoms like fatigue. But unlike most types of arthritis, it’s not a lifelong condition, and it usually lasts for less than a year.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Reactive arthritis happens when an infection in your urinary tract, genitals, digestive system or throat triggers an unusual reaction from your immune system. Your immune system normally generates inflammation to fight infections. But with Reiter’s syndrome, your immune system sends inflammation to places in your body where the infection never was. It’s as if it’s not convinced that the battle is over.
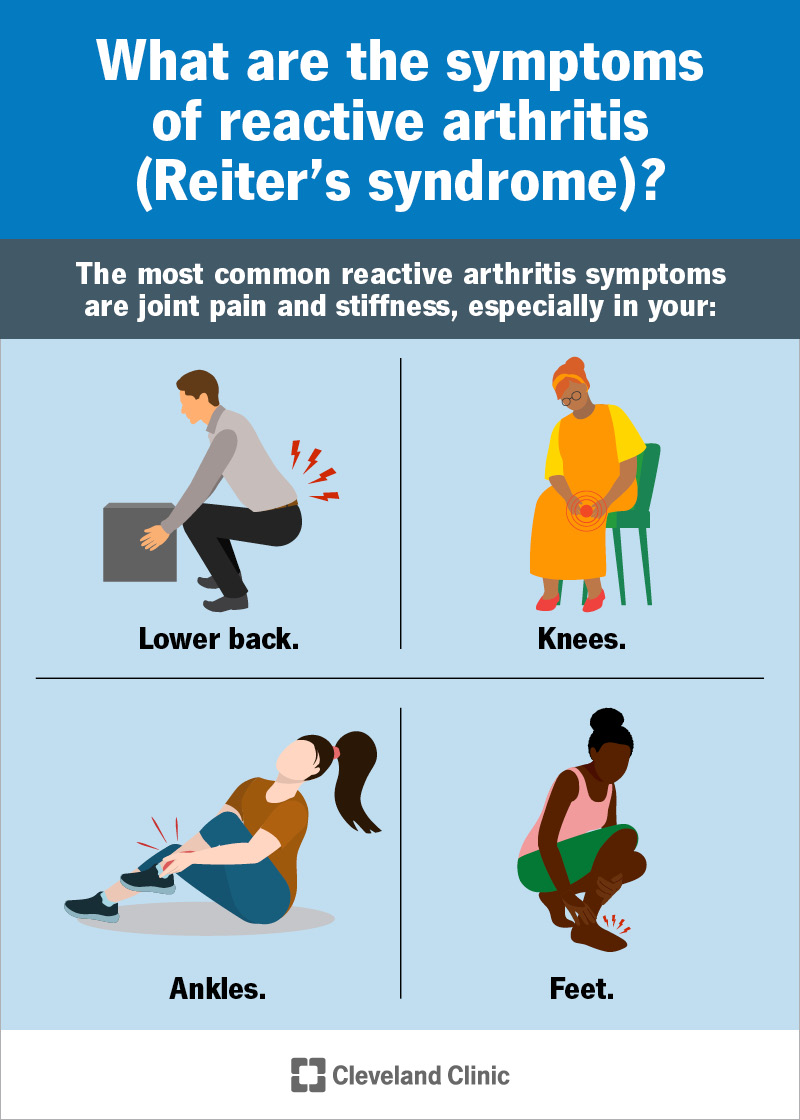
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/reactive-arthritis-reiters-syndrome.jpg)
The most common reactive arthritis symptoms are joint pain and stiffness, especially in your:
But you may also have a variety of other symptoms, including:
The classic triad of reactive arthritis symptoms is:
This triad makes for a quick way to recognize Reiter’s syndrome. But most people won’t have all of these symptoms at the same time. Different symptoms may come and go. You may never have the full triad, and you may also have other symptoms not listed in the classic triad.
Advertisement
Reactive arthritis starts with a bacterial infection. It’s usually a:
Some of the specific bacteria that can trigger it include:
Reiter’s syndrome begins several days to weeks after the original infection ends, and only in a small percentage of people. It appears that the infection triggers an autoimmune response. This means your immune system overcorrects and begins to target healthy parts of your own body with inflammation. Fortunately, unlike most autoimmune diseases, reactive arthritis is usually a temporary condition.
Reactive arthritis belongs to a group of inflammatory arthritis conditions called spondyloarthritis. Most of these are autoimmune diseases. Scientists aren’t sure why some people get autoimmune diseases and others don’t. You don’t have to have a severe infection to trigger reactive arthritis. One possible factor is a gene called HLA-B27. Many people who get spondyloarthritis and Reiter’s syndrome have it.
Anyone can get reactive arthritis, but you’re more likely to get it if:
If you've recently developed symptoms of arthritis, your healthcare provider will want to see them and hear about them. Certain combinations of symptoms will suggest reactive arthritis. They’ll particularly want to know if you’ve recently recovered from an infection that might have triggered Reiter’s syndrome.
You might have a variety of tests to help make the diagnosis, including:
Treatment for reactive arthritis may include:
Advertisement
Reiter’s syndrome is usually self-limited, meaning it will clear up on its own in time (in three to 12 months). In the meantime, treatment can often repress symptoms and may help them to go away quicker. But reactive arthritis is an autoimmune disorder, and no autoimmune disorder is really curable. This means it’s always possible for symptoms to return — for example, if you get another infection.
In a small percentage of people, Reiter’s syndrome seems to trigger a more serious and lasting form of spondyloarthritis. They develop long-term joint inflammation that can do real damage over time. It’s unclear whether this is chronic reactive arthritis or whether, in this case, you’ve developed a different disease. One autoimmune disease can trigger another, and many people have more than one.
Even though it’s likely to be temporary, reactive arthritis can have a major impact on your day-to-day life while it lasts. Although many people have mild symptoms that come and go, others struggle with severe fatigue and discomfort. You might need to adjust your daily schedule or how you work during this time.
Your healthcare provider might recommend:
Advertisement
Just when you thought your infection was over, reactive arthritis appears as an unexpected and unwelcome encore. It can make the symptoms of the original infection return, along with other symptoms — particularly, joint inflammation. Whether it affects you a little or a lot, it’s hard to live like this not knowing when it will end. But for most people, it will end, and treatment can help until it does.
Advertisement

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
When you have an inflammatory or autoimmune condition, you need experts by your side. At Cleveland Clinic, we’ll create an individualized treatment plan for you.
