Osteomyelitis is a serious infection that happens when bacteria or fungi infect your bone marrow. Infections usually start on your skin at a wound or surgery site then spread to your bones through your bloodstream. It can cause permanent bone damage if it’s not treated right away. Visit a healthcare provider as soon as you notice any symptoms.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
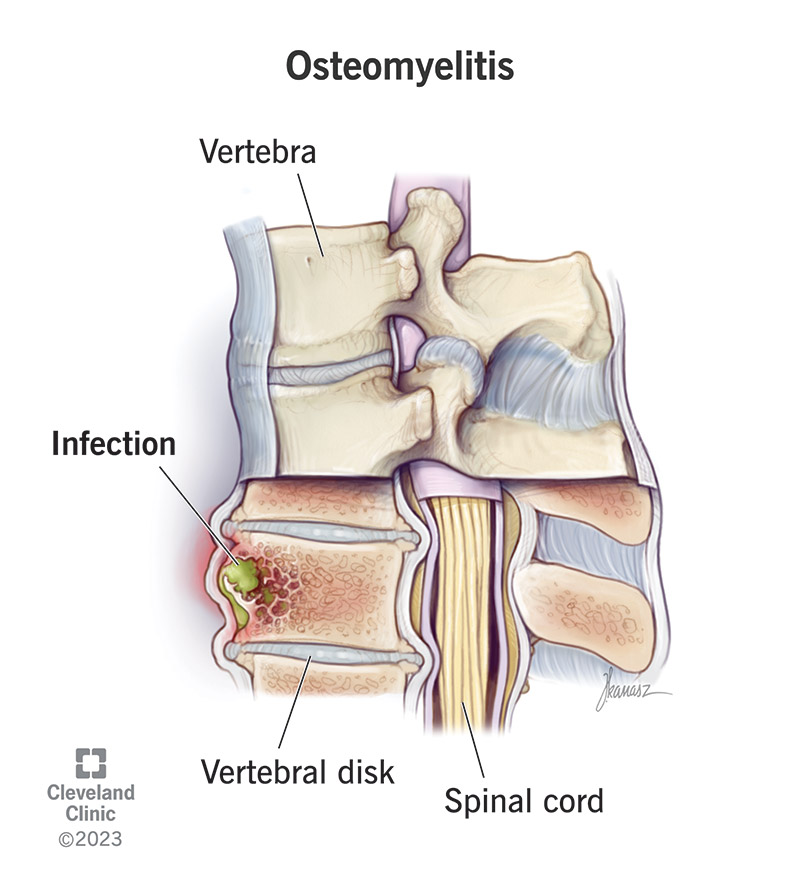
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/osteomyelitis)
Osteomyelitis is a bone infection. It happens when a bacterial infection or a fungal infection spreads to your bones.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Osteomyelitis causes painful swelling in your bone marrow. It can affect any of your bones. Kids with osteomyelitis most commonly have it in their leg or arm bones. Adults usually develop it in their vertebrae (the bones that make up your spine) or hips.
If it’s not treated in time, osteomyelitis can cause permanent bone loss and necrosis (tissue death).
There are a few types of osteomyelitis:
Researchers think fewer than 25 per 100,000 people experience osteomyelitis each year. However, some studies have found it’s much more common among people who need to stay in the hospital — as high as 1 out of every 675 hospital admissions.
Experts think this difference may be because people who are admitted to the hospital often have health conditions or injuries that make them much more susceptible to bacteria and fungi getting into their blood and bones.
Advertisement
Osteomyelitis symptoms can vary depending on which type you have and which of your bones are infected. The most common bone infection symptoms include:
Vertebral osteomyelitis also usually causes low back pain. Some people with chronic osteomyelitis don’t have symptoms.
Infections that spread to your bones cause osteomyelitis. It usually happens when an infection on the surface of your skin (like at a wound or a surgery site) gets into your bloodstream and spreads to your bone marrow (the spongy center of some bones).
Anyone can develop an infection that causes osteomyelitis, but some people have a higher risk, including people who:
People with health conditions or who need treatments that weaken their immune system are more likely to develop osteomyelitis, including:
Osteomyelitis complications can include:
A healthcare provider will diagnose osteomyelitis with a physical exam and some tests. They’ll ask about your symptoms and when you first noticed them. Tell your provider if you’ve recently had surgery, an injury or if you’ve started new treatments for other health conditions.
Your provider will use some of the following tests to diagnose the infection and take pictures of your bones:
Advertisement
Your provider will suggest treatments to kill the infection and prevent permanent bone damage. The most common osteomyelitis treatments include:
It can take a long time for osteomyelitis to heal. You might need antibiotics or antifungals for a few months. You should start feeling better as medications start killing the infection and slowing its spread.
Advertisement
Ask your provider how long you’ll need to take antibiotics or antifungals. Make sure you take the full dose they prescribe for as long as they say, even if you start feeling better.
Most people with osteomyelitis recover without long-term complications. But it’s important to get the infection diagnosed and start treatment right away. Contact your provider as soon as you notice any signs of an infection.
Osteomyelitis can last for a long time. You might need treatment for several months to make sure the infection is completely cured. Ask your provider or surgeon what to expect.
Cleaning new wounds or cuts and keeping surgery sites sterile are the best ways to prevent bone infections. Wash your hands frequently, and clean scrapes and cuts with warm, soapy water. Go to the emergency room if you have a deep cut or puncture (stab) wound or experience trauma.
Ask your provider how to clean your surgery site after any type of procedure.
Make sure you take the full course of your antibiotic or antifungal medication exactly as your provider prescribes. You need to finish the full dose, even if you feel better. If you stop taking your medications before you should, there’s a chance they won’t completely kill the infection. This increases your risk of chronic osteomyelitis and other complications.
Advertisement
Ask your surgeon how to keep incisions clean after surgery. They’ll tell you when it’s safe to shower or bathe, how to clean your surgical site and which kind of soap is best to use on it.
Contact your healthcare provider or surgeon right away if you notice signs of an infection, especially at a surgery site.
Contact your provider or surgeon right away if you notice signs of an infection, especially if you notice pus or discharge at a wound or surgery site.
You may want to ask your provider:
Osteomyelitis is a serious condition that needs treatment right away. It usually responds very well to treatment, but you need to start treating it as soon as possible to prevent serious complications.
Once a provider diagnoses the infection and you start treatment, try not to worry. It might take a while to cure the infection, but the most important part is catching osteomyelitis early.
No, osteomyelitis won’t go away on its own. It’s extremely important to see a healthcare provider for a diagnosis and treatment. Your immune system does an amazing job of fighting off germs and other invaders, but you need antibiotics or antifungals to kill the infections that cause osteomyelitis.
Never ignore signs of infection around a wound, especially if you just had surgery. Contact your provider or surgeon right away if you notice any changes in your incisions. It’s always better to ask too many questions than not enough. Trust your instincts — if something doesn’t look or feel right, it’s worth checking out.
Osteomyelitis is a bone infection that happens when bacterial or fungal infections spread from other parts of your body into your bone marrow. It can be very serious and cause permanent bone damage, but it’s very manageable if you start treatment within a few days. Contact a healthcare provider right away if you notice signs of infection like a feeling of warmth, pus or discharge or if you have a fever.
It’s especially important to keep your incisions clean after having surgery. Your surgeon will give you specific instructions on how to keep your surgery site clean. Don’t be afraid to ask lots of questions. Your providers are there to help you stay safe and healthy; they won’t be upset to explain things in a different way or show you exactly what you need to do.
Learn more about the Health Library and our editorial process.
Cleveland Clinic's health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability, and up-to-date clinical standards.
Cleveland Clinic's health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability, and up-to-date clinical standards.
From sudden injuries to chronic conditions, Cleveland Clinic’s orthopaedic providers can guide you through testing, treatment and beyond.
