Vertebral osteomyelitis is a rare infection in your spine. It happens when bacteria or fungi infect your vertebrae (spine bones). The infection can start in your spine if the germs get in a wound or surgery site. It can also spread to your spine from somewhere else in your body. You’ll need medication for several weeks to kill the infection.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
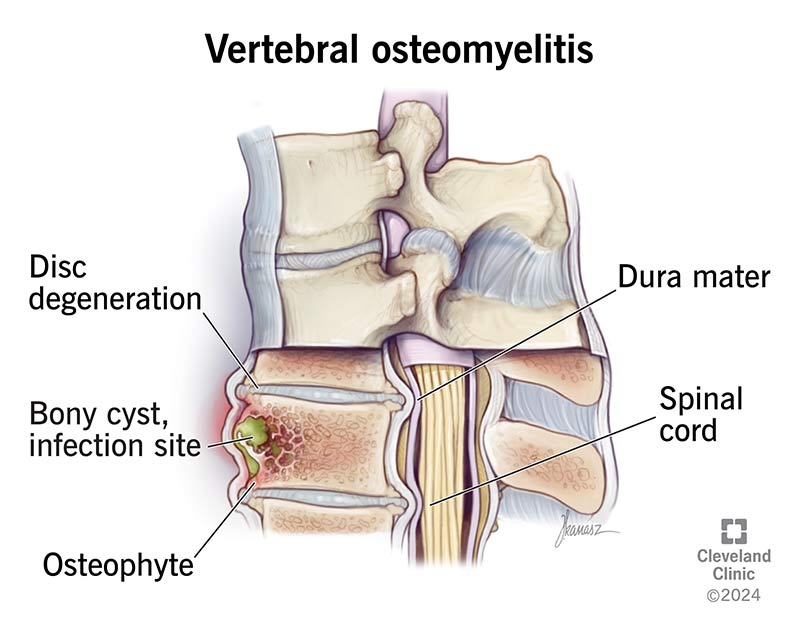
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/22276-vertebral-osteomyelitis-spine)
Vertebral osteomyelitis is a rare spine infection. It happens when there’s a bone infection (osteomyelitis) in one of the bones in your spine (vertebrae).
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Vertebral osteomyelitis can happen as the result of a spine injury or after surgery. It can also spread to your spine from another place in your body. Other names for this condition include spinal osteomyelitis and spondylodiskitis.
See a healthcare provider right away if you think you might have vertebral osteomyelitis. It can be fatal if it’s not treated.You’ll need medication to treat the infection and other treatments to manage symptoms or complications you experience.
Symptoms of vertebral osteomyelitis can include:
You might feel back pain in one spot (localized) or it might spread (radiate) to other parts of your body. It’s most common to feel pain in your lower back (lumbar spine).
It’s common to have a fever when you have an infection. But you probably won’t if you have vertebral osteomyelitis. Experts estimate that only around 1 in 3 people with vertebral osteomyelitis have a fever they can feel or notice.
Infections that affect your spinal bones cause vertebral osteomyelitis. Bacterial infections are the most common cause, especially staph infections and MRSA. It’s much less common, but some fungal infections can also cause it.
Advertisement
You might have an open wound near your spine after an injury, spine injection or spinal surgery that lets germs in. Or an infection somewhere else in your body can spread to your spine through your bloodstream.
Anyone can get vertebral osteomyelitis, but you may be more likely to if you:
You might have a higher risk if you have a condition or need treatments that weaken your immune system. Examples include:
Vertebral osteomyelitis complications can include:
A healthcare provider will diagnose vertebral myelitis with a physical exam and some tests.
Your provider will examine your back and spine. Tell them when you first noticed pain and other symptoms (especially if certain activities or movements make them worse).
There are a few tests your provider can use to diagnose vertebral osteomyelitis and the infection that caused it. You might need:
Your healthcare provider will prescribe medication to kill the infection. You’ll need antibiotics if you have a bacterial infection or an antifungal if you have a fungal infection.
Make sure to take your medication for as long as your provider says (even if you start feeling better sooner). If you don’t take the full course, it won’t kill all the bacteria or fungi. This can let the infection come back (recur). Infections that recur are often more severe and have a higher risk of complications.
Your provider might suggest other treatments, including:
Advertisement
Vertebral osteomyelitis symptoms can be hard to notice. That’s because back pain is an extremely common issue.
Visit a healthcare provider if you have pain that lasts for more than a few days — especially if rest or other at-home treatments don’t help you feel better. Talk to your provider right away if you notice any changes in your ability to feel or move any part of your body.
Vertebral osteomyelitis is a serious infection that can be fatal.
With treatment, you may recover from vertebral osteomyelitis in about four to six weeks. However, it might take up to six months to feel fully recovered.
Without treatment, you may develop severe spine damage or blood poisoning (septicemia). Experts estimate that around 1 in 10 people with vertebral osteomyelitis die within a year even though they’ve received a diagnosis and treatment and have gotten better.
Thinking about an infection in your spine, like vertebral osteomyelitis, can be scary. But it’s treatable, so don’t hesitate to see a healthcare provider if you think something is wrong. Trust your intuition. You know when pain, weakness or other symptoms aren’t right. The faster a provider can diagnose vertebral osteomyelitis and prescribe medication to treat it, the better.
Advertisement

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Back pain can stop you in your tracks. But you don’t have to live like that. Cleveland Clinic is here to help you get moving again.
