Arthroplasty is surgery to replace all or some of a joint. Your surgeon will replace worn-out or damaged bone and cartilage in your natural joint with a prosthetic implant. It usually takes at least a few months to recover after an arthroplasty. Your recovery time will depend on which joint needs a replacement.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
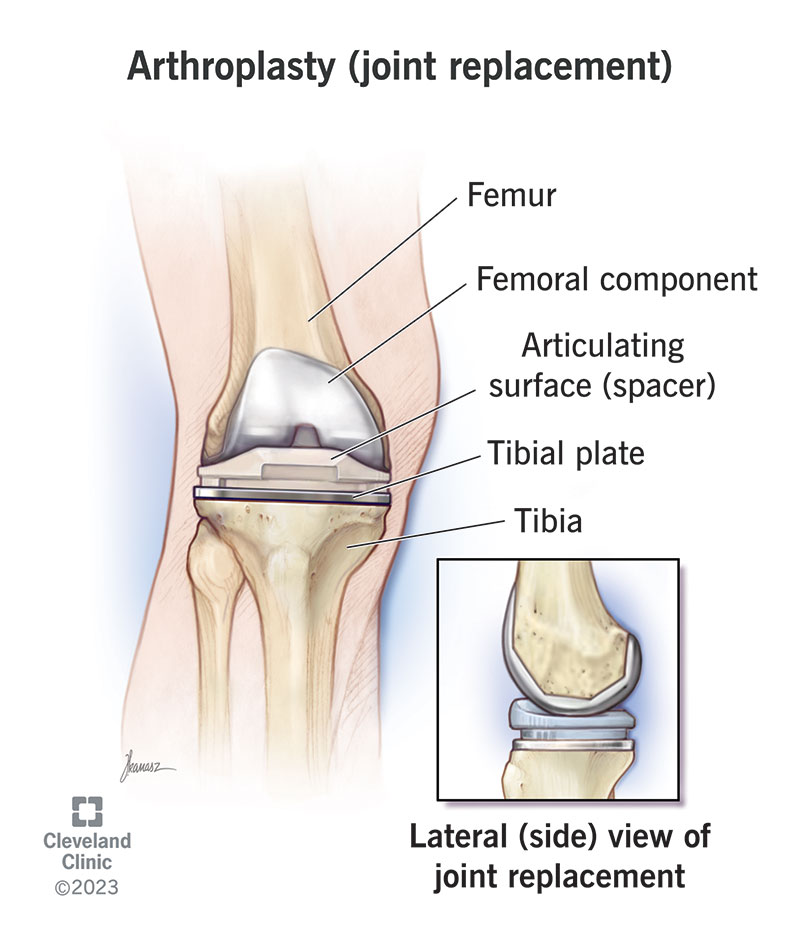
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/arthroplasty)
Arthroplasty is a surgical procedure to replace some or all of a joint. Healthcare providers also call it joint replacement surgery or joint replacement.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
A surgeon will remove the worn-out or damaged parts of your natural joint and replace them with an artificial joint (a prosthesis) made of metal, plastic or ceramic.
Any large joint can be replaced with an arthroplasty, including your:
Your surgeon will suggest either a total or a partial joint replacement:
A healthcare provider might recommend joint replacement surgery if you have severe symptoms that don’t get better after trying nonsurgical treatments like activity modifications, physical therapy or medications. Symptoms that can cause you to need an arthroplasty can include:
Advertisement
Arthritis is the most common reason people need an arthroplasty. Most people who choose to have a joint replacement have osteoarthritis, but some people with rheumatoid arthritis may need one, too.
A healthcare provider might suggest an arthroplasty if you’ve experienced a bone fracture (broken bone) in your joint or if you have post-traumatic arthritis. Trauma that causes fractures or post-traumatic arthritis can include:
Arthroplasties are some of the most common surgeries. Surgeons perform more than 850,000 knee replacements and more than 450,000 hip replacements every year in the U.S.
Your healthcare provider or surgeon will help you get ready for surgery. You might need:
Tell your provider and surgeon about any medications and over-the-counter (OTC) supplements you take. You may have to stop taking them before your surgery.
Your surgeon will tell you when you should stop eating and drinking the day before your surgery. Most people need to avoid eating and drinking for eight hours before their surgery. Your surgeon will tell you which medications are safe to take with a sip of water the morning of your surgery.
The day of your surgery you’ll receive anesthesia to numb your body and make sure you don’t feel any pain. An anesthesiologist will give you either general anesthesia to put you to sleep during your surgery or regional anesthesia to numb the area around your joint that needs replacing. They may give you other medications to make you sleep if you need regional anesthesia.
During a joint replacement, your surgeon will:
Some types of arthroplasties can be done as robotic-assisted joint replacements. This doesn’t mean a robotic surgeon does the procedure automatically — it’s a special technique to help your surgeon. During a robotic-assisted arthroplasty, your surgeon will use a special computer that guides their surgical tools during the operation. Studies have found that robotic-assisted joint replacements can be more accurate and insert prosthetic implants more securely.
Advertisement
It’s most common for surgeons to use robotic assistance to replace bigger joints like hips and knees.
Arthroplasties usually take a few hours from start to finish. It depends on which of your joints needs a replacement, and if you’re getting a total or partial joint replacement.
After surgery, you’ll be moved to a recovery room. Your surgery team will keep an eye on you for a few hours to make sure you wake up from the anesthesia without complications. They’ll also monitor your vital signs and pain level.
Some people who have joint replacement surgery go home the same day. You might need to stay in the hospital overnight or for a few days. Your surgeon will tell you when it’s safe for you to go home.
For most people, the benefits of a joint replacement far outweigh the risks. An arthroplasty is a major surgery, and that means there’s always a chance you experience complications. However, many people who have a joint replacement experience a big, noticeable improvement in their daily routines — especially if they’ve been living in pain for a long time.
Certain health conditions can make recovery from an arthroplasty more difficult. Talk to your surgeon about your health history. Tell them if you have:
Advertisement
Talk to your healthcare provider or surgeon about the risks of a joint replacement. They’ll help you decide if arthroplasty is right for you.
Arthroplasty is a safe, effective procedure that helps people regain their mobility and relieves long-term pain. Most people who have a joint replacement have an increased quality of life because they can move better with less pain.
Some people who have joint replacement surgery still experience pain and other symptoms in their affected joint. Rare complications include:
Your surgeon will tell you what you can expect after your surgery and how you can reduce your chances of experiencing complications.
It’s important to follow your surgeon’s and physical therapist’s recovery instructions and to avoid limping after your surgery. Moving unusually or unnaturally can cause tendinitis or bursitis.
A joint replacement usually lasts a long time. Many people who have a joint replacement live with it for the rest of their lives.
Advertisement
It’s rare, but some people need additional surgeries on that same joint in the future. Your surgeon will tell you what to expect.
It depends on which joint was replaced. It usually takes at least a few months to recover after an arthroplasty. Everyone’s body responds differently to joint replacement surgery.
Your recovery time will depend on several factors, including:
Your surgeon will give you a customized recovery plan, but in general, you should:
After surgery, you’ll feel pain, especially in the first few weeks of your recovery. You’ll feel pain from the surgery itself and pain as your body begins to heal.
Your surgeon will suggest a combination of prescription pain medication, over-the-counter nonsteroidal anti-inflammatory drugs (NSAIDs) — if it’s safe for you to take them — and acetaminophen to relieve your pain. Your surgeon will tell you how much of each kind of medication you can take each day or in a certain amount of time.
Talk to your surgeon if you feel like you’re experiencing too much pain or if you’re worried about any complications from taking pain medication.
Ask your surgeon or physical therapist for tips to move through your home safely after your surgery. They can show you how to safely:
How long you’ll need to miss work or school depends on how much stress your job or other activities put on your affected joint. Most people need to rest at home for a few weeks. Your surgeon will tell you when it’s safe to return to work or school.
Call your surgeon or healthcare provider right away if you experience any of the following symptoms:
Choosing to have an arthroplasty (joint replacement surgery) is a big decision. Talk to your healthcare provider and surgeon before you decide to have a joint replacement. Most people who have an arthroplasty experience a noticeable improvement in their quality of life. Joint replacements can relieve symptoms like pain, stiffness and difficulty moving.
After your surgery, you’ll need time to strengthen your muscles and heal your body. Take your recovery slow and don’t rush yourself. Talk to your surgeon or physical therapist about your movement goals and which activities you’d like to participate in after your joint replacement.

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Stiff, painful joints don’t have to slow you down for good. Cleveland Clinic’s joint replacement surgery experts can help you get back to doing what you love.
