Aortic regurgitation describes an aortic valve (between your main artery and main pumping chamber) that doesn’t close tightly. Blood leaks backward with each heartbeat. You may have no symptoms from this heart valve disease at first. But as the condition worsens, you may have chest pain, shortness of breath or palpitations.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
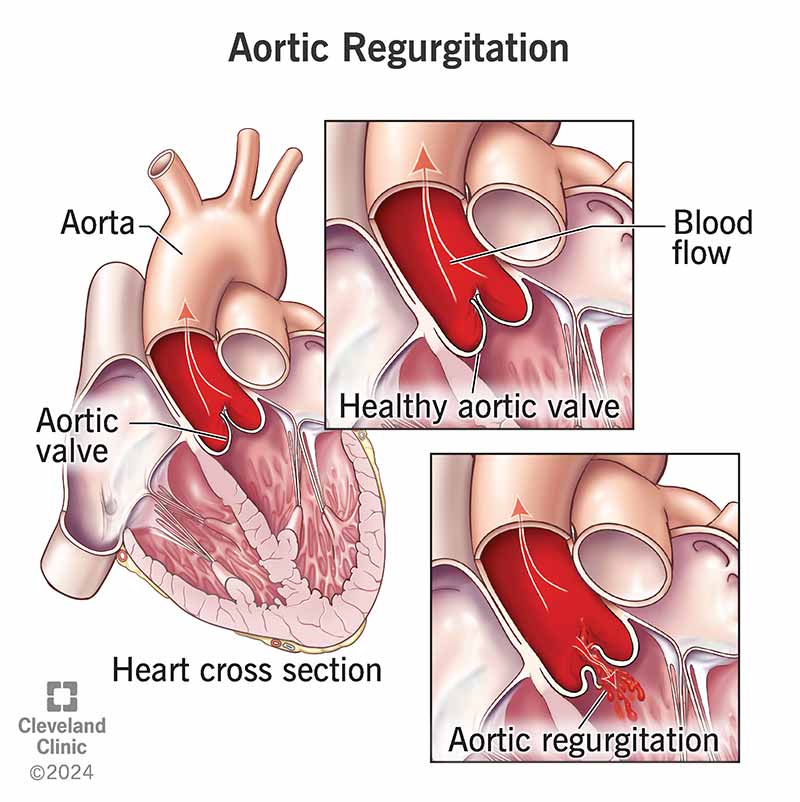
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/aortic-regurgitation)
Aortic regurgitation refers to a leaky aortic valve. With this condition, the leaflets or cusps of your heart’s aortic valve don’t close as tightly as they should. As a result, some blood that should move out of your heart leaks backward each time your heart beats.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Your aortic valve is the “door” that opens and closes to control blood flow between your heart and your aorta (the largest artery in your body). With each heartbeat, your heart pumps oxygen-rich blood into your aorta. From there, your blood then travels through many branches to reach your organs and tissues.
Your aortic valve opens to allow blood to travel from the left ventricle of your heart (its main pumping chamber) into your aorta. This happens each time your left ventricle contracts (squeezes). When your left ventricle relaxes, the valve closes.
Normally, your aortic valve closes tightly enough to keep blood flowing in the correct direction. But if you have aortic valve regurgitation, your valve doesn’t close all the way. This means that each time your left ventricle relaxes, some blood leaks backward into this chamber. While this is a cause for concern, healthcare providers have treatments they can use to help you.
Aortic regurgitation is a common form of heart valve disease that ranges from mild to severe. Providers also call this condition aortic insufficiency.
Healthcare providers separate aortic regurgitation into two types:
Advertisement
Providers may also refer to aortic valve regurgitation as one of three (1, 2 or 3) types based on detailed descriptions of the issue. They may also talk about different stages (A, B, C or D) based on severity. Stage D is the most severe.
Aortic regurgitation symptoms include:
Chronic, mild aortic regurgitation may not cause any symptoms for a long time. As your condition gets worse, you may gradually develop symptoms.
Aortic regurgitation causes include:
Certain changes to your aortic valve anatomy and other medical conditions make you more likely to develop a leaky aortic valve. You’re at risk for aortic valve regurgitation if you have:
A leaky aortic valve causes extra blood to flow into your left ventricle. This means the pumping chamber has too much blood to handle (volume overload). It makes your left ventricle do more work to manage this extra blood volume and pump enough blood into your aorta.
Over time, this can cause the muscular walls of your left ventricle to thicken and dilate (left ventricular hypertrophy). This makes your heart less efficient. Other complications may include heart failure and arrhythmia.
Advertisement
Acute aortic regurgitation can cause pulmonary edema (fluid in your lungs) and lower your cardiac output.
Healthcare providers diagnose aortic valve regurgitation through a physical exam and testing.
During a physical exam, your provider:
A wide pulse pressure (40+ mmHg) could mean a leaky aortic valve.
An echocardiogram (echo) is the gold standard for diagnosing aortic regurgitation. This test uses high-frequency sound waves (ultrasound) to take pictures of your heart. Your provider can use different techniques, like Doppler ultrasound, to check your valve function. Doppler ultrasound shows the speed and direction of blood flow through your heart.
Other tests you may need to diagnose aortic regurgitation or plan treatment include:
Aortic regurgitation treatment may include medication or surgery. If you have an acute case, you’ll need treatment right away.
Advertisement
Depending on the severity of your condition, you may need surgery to repair or replace your aortic valve. Your healthcare provider will evaluate you and decide if you need surgery. They’ll consider whether the benefits of surgery outweigh its potential risks for you. Many things can raise your surgical risks or complicate healing, including tobacco use and unmanaged underlying conditions. Your provider will talk with you about your risks and whether it’s safe to proceed with surgery.
If valve surgery isn’t a good option for you, your provider may prescribe medications to manage heart failure and improve your quality of life. Other medicines may reduce your risk of blood clots and stroke. Medicines help with your symptoms, but they can’t keep severe aortic regurgitation from getting worse or cure it.
People who get an aortic valve repair or replacement may need another surgery in the future. There are also risks of:
After an aortic valve replacement, you might need to take anticoagulants to prevent blood clots. You’ll need to take them for a few months (for bioprosthetic valves made from pig, cow or human tissue) or for the rest of your life (for mechanical valves). In some cases, replacement valves may move out of place or leak.
Advertisement
If you get a new valve, your provider may recommend that you take antibiotics before visiting the dentist. This can prevent endocarditis (infection inside your heart).
You can have chronic aortic regurgitation for several years without having symptoms. But it can get worse over time. You may suspect it’s happening if you start having shortness of breath or chest pain.
Your outlook depends on many factors. These include:
Research shows that people who have valve replacement surgery before developing heart failure have a good long-term prognosis (outlook), even if their cases were severe. People who’ve developed heart failure may have a worse prognosis.
People with mild to moderate aortic regurgitation do well after treatment. They have a 10-year survival rate of 80% to 95%.
It’s important to talk to your healthcare provider about your outlook. Your provider knows you and your medical history best, and they can use this information to give you an idea of what to expect.
You can’t always prevent heart valve disease. But you can lower your risk by:
Follow your healthcare provider’s guidance on self-care, including medications and lifestyle changes. In general, it’s important to take all of your medications as prescribed and at the same time each day. Your provider may also advise you to change some habits, including:
If you have aortic regurgitation, it’s crucial to keep up with your medical appointments so your provider can keep an eye on your condition. Your provider will tell you how often you need to come in.
You’ll need echocardiograms at regular intervals (anywhere from every six months to every five years) so your provider can check your valve and heart function. Regular visits are essential so your provider can catch signs of worsening aortic regurgitation. This allows you to receive treatment at the right time and avoid permanent damage to your heart.
If you’ve had heart valve surgery, be sure to stick to the follow-up schedule your provider gives you. Your provider will monitor you closely to make sure your heart is working well and you don’t develop heart failure or other issues.
Call your provider any time you have new symptoms, worsening symptoms or questions about your condition.
Call 911 or your local emergency number if you have symptoms of a heart attack or stroke. These are life-threatening emergencies that require immediate medical care.
Living with heart valve disease can be stressful. You may have lots of questions about your condition but not know where to start. Here are a few questions you can ask your provider to begin learning more:
More than 25% of people with left ventricle dysfunction start to have symptoms within one year. In a study of people with mild or moderate aortic regurgitation, most people didn’t get worse (progress). The study did follow-ups with people for about five years.
Aortic regurgitation can be life-threatening if it’s severe and acute (coming on suddenly). It can lead to heart failure, myocardial ischemia (not enough blood reaching your heart muscle) or sudden death. You need surgery right away if you have symptoms with severe acute regurgitation.
Learning you have a leaky aortic valve can feel scary, and you may wonder what the future will bring. The good news is that advances in medicine can help many people with aortic regurgitation. Talk to your provider about treatment options and which ones may be best for you.

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
When you have aortic heart valve disease, you want the best care. Cleveland Clinic is number one in the nation for heart health. We’re ready to help you.
