Healthcare providers use vagal maneuvers as a first-choice option for certain people whose heart rate is too fast. It has less risk and a lower cost than other treatments. If vagal maneuvers don’t work, healthcare providers will use medical or electrical cardioversion to put your heart back in a normal rhythm.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
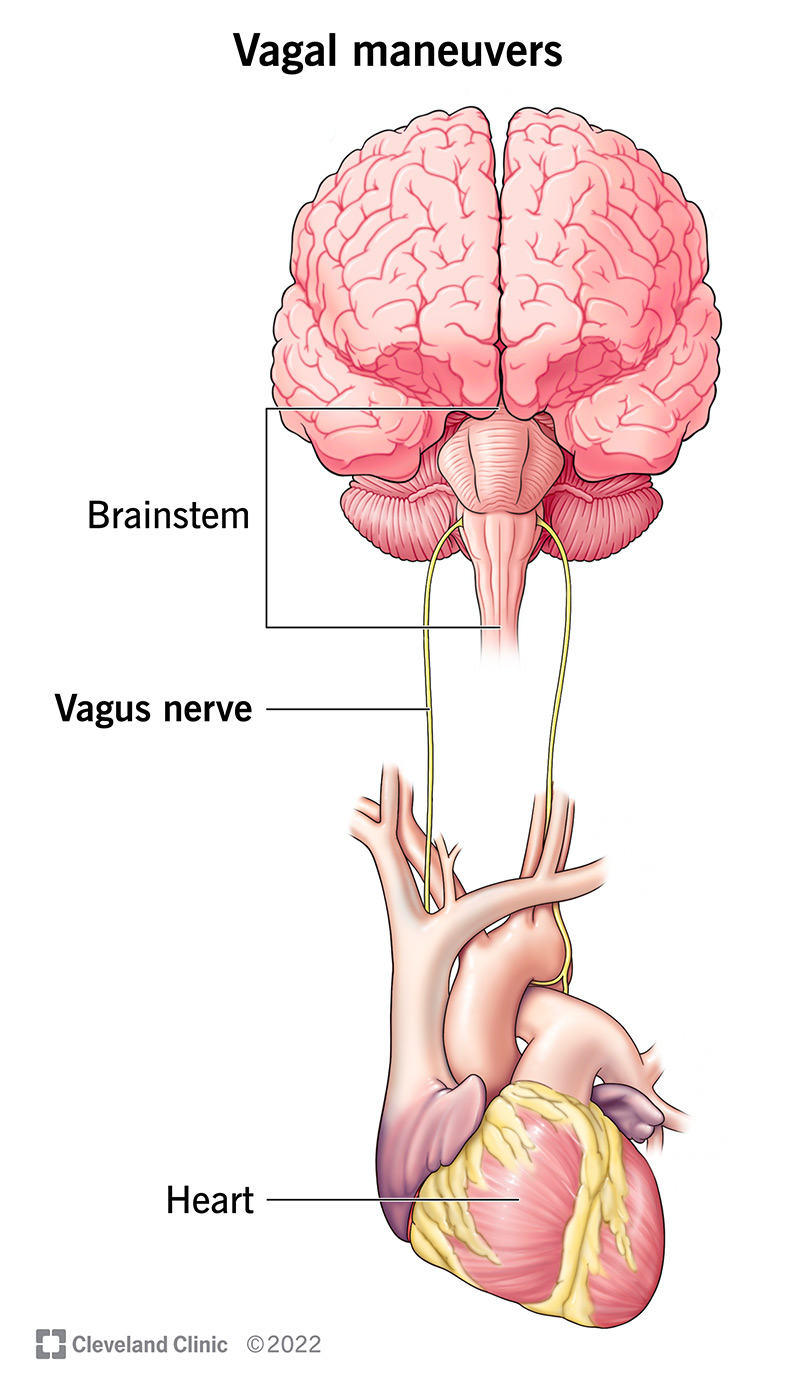
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/22227-vagal-maneuvers)
Vagal maneuvers are physical actions that make your vagus nerve act on your heart’s natural pacemaker, slowing down its electrical impulses. Your vagus nerve — which goes from your brainstem to your belly — plays a major role in your parasympathetic nervous system, which controls a number of things in your body, including heart rate.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Healthcare providers can do vagal maneuvers when it makes sense for a person with a fast heart rate. Don’t try these yourself without talking to your healthcare provider first.
Healthcare providers often use these:
Vagal maneuvers are a first-line (first choice) treatment for supraventricular tachycardia (SVT) (fast heart rate) because they’re a low-risk, low-cost way to slow down a heart rate that’s too fast. They can have a 20% to 40% success rate for getting certain fast heart rhythms (more than 100 beats a minute) back to normal rhythms.
Vagal maneuvers can also help your healthcare provider diagnose which type of arrhythmia (irregular or abnormal beat) you have, as certain types of heart rhythm disorders classically respond to this maneuver.
Your healthcare provider will only use vagal maneuvers if you’re considered stable. They won’t do vagal maneuvers if you’re unstable, meaning you have:
Advertisement
If you’re unstable, your healthcare provider will do cardioversion (using medicine or an electrical shock) instead of vagal maneuvers. Anyone who’s feeling unwell should go to an emergency room or call 911 immediately.
Supraventricular tachycardia (SVT) is common in adults and children, and is the most common heart rhythm abnormality in children. An estimated 1 in 250 to 1 in 1,000 children have SVT. Since vagal maneuvers are the first treatment choice for SVT, they’re commonly used.
Your healthcare provider will do an electrocardiogram (EKG) to check your heart rhythm. They’ll monitor your heart rate, blood pressure and oxygen level.
Here’s how healthcare providers do the three most common vagal maneuvers:
While sitting, you’ll take several deep breaths, hold your breath and then quickly put your whole face into a container of ice water. Keep your face submerged as long as you can.
The alternative approach is putting a bag of ice water or an ice-cold, wet towel against your face.
While lying on your back, take a deep breath and act like you’re exhaling but with your nose and mouth closed for 10 to 30 seconds. It should feel like trying to breathe air out into a blocked straw.
In a modified version of this maneuver (which can work better than the original method), you can do this while sitting up and then have your healthcare provider quickly drop the part of the bed supporting your upper body.
When they lower your bed, they bring your knees to your chest or put your legs in the air. Keep your legs in that position 30 to 45 seconds longer than holding your breath.
Another Valsalva technique healthcare providers use for kids is to have them blow on their thumb without letting any air out.
You’ll lie on your back with your head turned to one side. Your healthcare provider will use their fingers to push on your carotid sinus for five to 10 seconds. If it doesn’t work, they can try again after a minute or try the other side of your neck.
Hopefully, the arrhythmia (irregular or abnormal beat) resolves. Your healthcare provider will do another electrocardiogram (EKG) to see if the vagal maneuver was successful at bringing your heart rhythm back to normal. If they try vagal maneuvers two or three times and they don’t work, they can give you medication to treat your arrhythmia. Medical or electrical cardioversion is another treatment option.
If vagal maneuvers don’t work, your healthcare provider may contact a cardiologist (heart specialist) to evaluate you.
Advertisement
Vagal maneuvers can help people with supraventricular tachycardia get their heart rhythm back to normal. They’re also less expensive and safer than treatments like medication or cardioversion. They don’t require any drugs, either.
Complications rarely happen when healthcare providers use vagal maneuvers on people who are a good fit for the procedures. Most complications don’t last long. They include:
With the diving reflex maneuver, there’s a risk of people breathing in ice water and drowning.
Carotid sinus massage can have rare, temporary complications. The risk of stroke from carotid sinus massage is 1 in 1,000. Healthcare providers don’t recommend carotid sinus massage for people who:
Vagal maneuvers can slow down a supraventricular tachycardia (SVT) (fast heart rate) 20% to 40% of the time. However, if you have a fast heart rate again and again, your healthcare provider may prescribe medication for you and/or recommend other treatment, such as catheter ablation. They may also teach you how to do vagal maneuvers on your own.
Advertisement
If you’re having chest pain or other symptoms of a heart attack, you should call 911.
You should contact your healthcare provider if you have questions about your diagnosis or treatment for supraventricular tachycardia.
Vagal maneuvers can help some people get their heart back to a normal rhythm, but they aren’t for everyone. It’s important to contact your healthcare provider before trying them on your own. They can teach you how to do them safely. If vagal maneuvers don’t work, you may need to take medication. Follow your healthcare provider’s instructions for taking any medication. It’s also important to go to all follow-up appointments with your healthcare provider.
Advertisement

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
When your heart rhythm is out of sync, the experts at Cleveland Clinic can find out why. We offer personalized care for all types of arrhythmias.
