PSVT is a type of arrhythmia. It causes a fast heart rate and other symptoms, like chest discomfort, heart palpitations, shortness of breath and dizziness. These symptoms start and end abruptly, sometimes with no clear trigger. A procedure called catheter ablation can cure PSVT and keep episodes from coming back.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
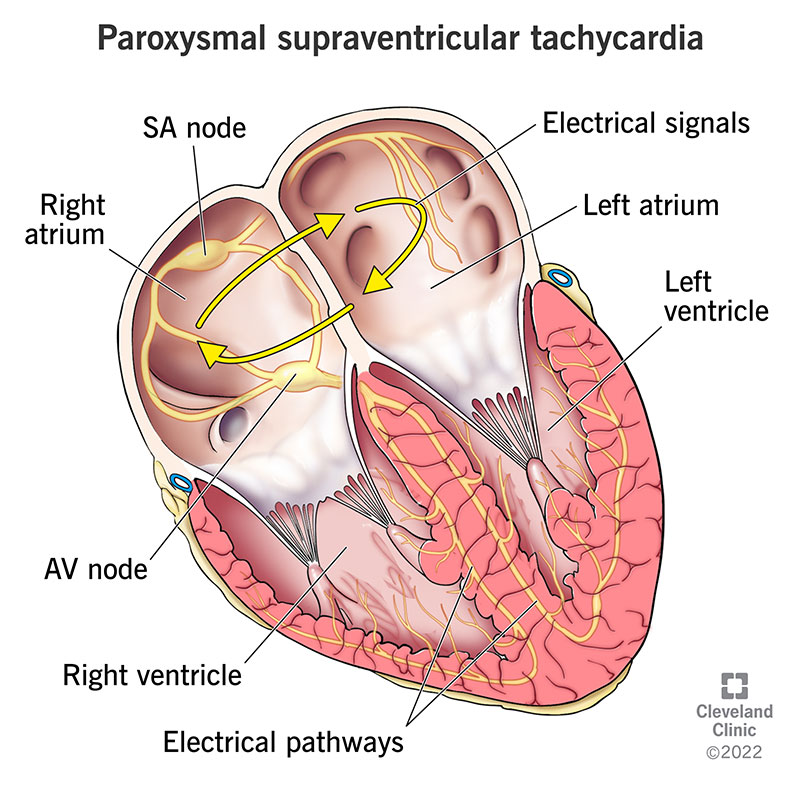
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/22232-paroxysmal-supraventricualar-tachycardia-psvt)
PSVT stands for paroxysmal supraventricular tachycardia. There are multiple types of this arrhythmia, or abnormal heartbeat, but they all start in the upper part of your heart. You have episodes where your heart beats very fast. These episodes start and end abruptly. Each episode may last for just a few seconds, several minutes or many hours.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
You don’t always need treatment, and the condition usually isn’t life-threatening. If needed, providers can treat PSVT with medicines or procedures.
When you’re learning about PSVT, it can help to know what each part of the name means:
PSVT is defined by its “paroxysms,” or abrupt episodes.
This condition affects about 168 to 332 out of every 100,000 people in the U.S. It’s diagnosed in people of all ages.
There are a variety of arrhythmias that healthcare providers would consider PSVT. The most common ones include:
Advertisement
PSVT is an episode where your heart beats very fast — over 100 beats per minute (bpm). Your heart rate may even reach 200 bpm or higher. The faster your heart rate, the more likely you are to have other symptoms, like:
These symptoms may stop on their own. In some cases, you may need treatment to stop an episode.
Abnormal electrical activity in your heart causes PSVT. This usually means electrical signals are doing one of the following:
These electrical issues won’t cause symptoms all the time. Instead, you’ll have episodes that come and go. What triggers an episode can vary from person to person, but may include:
Sometimes, there’s no clear trigger.
Certain medications can rarely increase your risk, particularly if they cause changes to your electrolytes, hormones, such as thyroid, or adrenaline. Check with your provider if any of your medications need to be adjusted.
PSVT can damage your heart if it happens often, leading to dilated cardiomyopathy. When this happens, healthcare providers call it “arrhythmia-induced cardiomyopathy.” The good news is that treating the arrhythmia can often reverse some or all of the damage.
Your healthcare provider will perform a physical exam and ask you some questions. You’ll talk about:
Tests that check your heart’s electrical activity are key to making a PSVT diagnosis. For example, an EKG in your provider’s office is often the starting point. This can be very helpful. But it may not capture the fast heartbeat as it’s happening.
That’s why your provider may suggest ambulatory monitoring. This means you wear a device as you go about your daily life. It saves data for your provider to review and often reveals things that an EKG didn’t.
Other tests you may need include:
Not everyone with PSVT needs treatment. But your provider may recommend treatment in certain situations — like if an episode doesn’t go away on its own, or if you have frequent or severe symptoms.
Treatments to stop an episode when it’s happening (acute therapy) include:
Advertisement
Acute therapy may be all you need. But if PSVT disrupts your life or puts you at risk of heart problems, you may need catheter ablation. This procedure creates helpful scar tissue in your heart to block abnormal signals. Ablation is safe and highly successful for most people and, depending on the type of PSVT, can frequently cure it.
In certain situations, providers recommend taking medicine long-term instead of ablation. They may prescribe beta-blockers or calcium channel blockers for you to take. You may take your medicine all the time or only as needed (the “pill-in-the-pocket” approach). You’ll work with your provider to decide the best plan to meet your needs.
Advertisement
Talk to your provider if you have any concerns about your heartbeat or any symptoms of PSVT. If you have PSVT, you’ll see your heart doctor for routine checkups and tests.
Seek medical care right away if:
Your prognosis depends on the treatments you receive and whether you have other heart problems. Ablation could cure your PSVT so you won’t have to deal with symptoms anymore. Symptoms are more likely to come back at least once a month if you take medicines but don’t do ablation.
When your heart starts racing, it can get your mind racing, too. PSVT might make you worry about your heart and wonder when the next episode will strike. But you don’t have to keep dealing with it. Talk to your healthcare provider about available treatments. They’ll help you understand your options and what you can expect.
Advertisement

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
When your heart rhythm is out of sync, the experts at Cleveland Clinic can find out why. We offer personalized care for all types of arrhythmias.
