AVNRT is a type of arrhythmia that makes your heart beat much faster than normal — typically 120 to 200 beats per minute. It’s not life-threatening, but it can cause symptoms that come and go suddenly. These episodes may disrupt your daily life. Treatments — including medicines and procedures — can reduce symptoms and prevent future episodes.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Atrioventricular nodal reentrant tachycardia (AVNRT) is a type of abnormal heartbeat (arrhythmia). You have episodes where your heart suddenly starts beating very fast — typically over 120 beats per minute. AVNRT is one of the most common types of supraventricular tachycardia (SVT), or fast heartbeats that begin in your heart’s upper chambers.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Here’s what each part of AVNRT means:
AVNRT can affect people at any age, but it often starts around age 30. It’s more common in females than in males. AVNRT can occur in young, otherwise healthy adults.
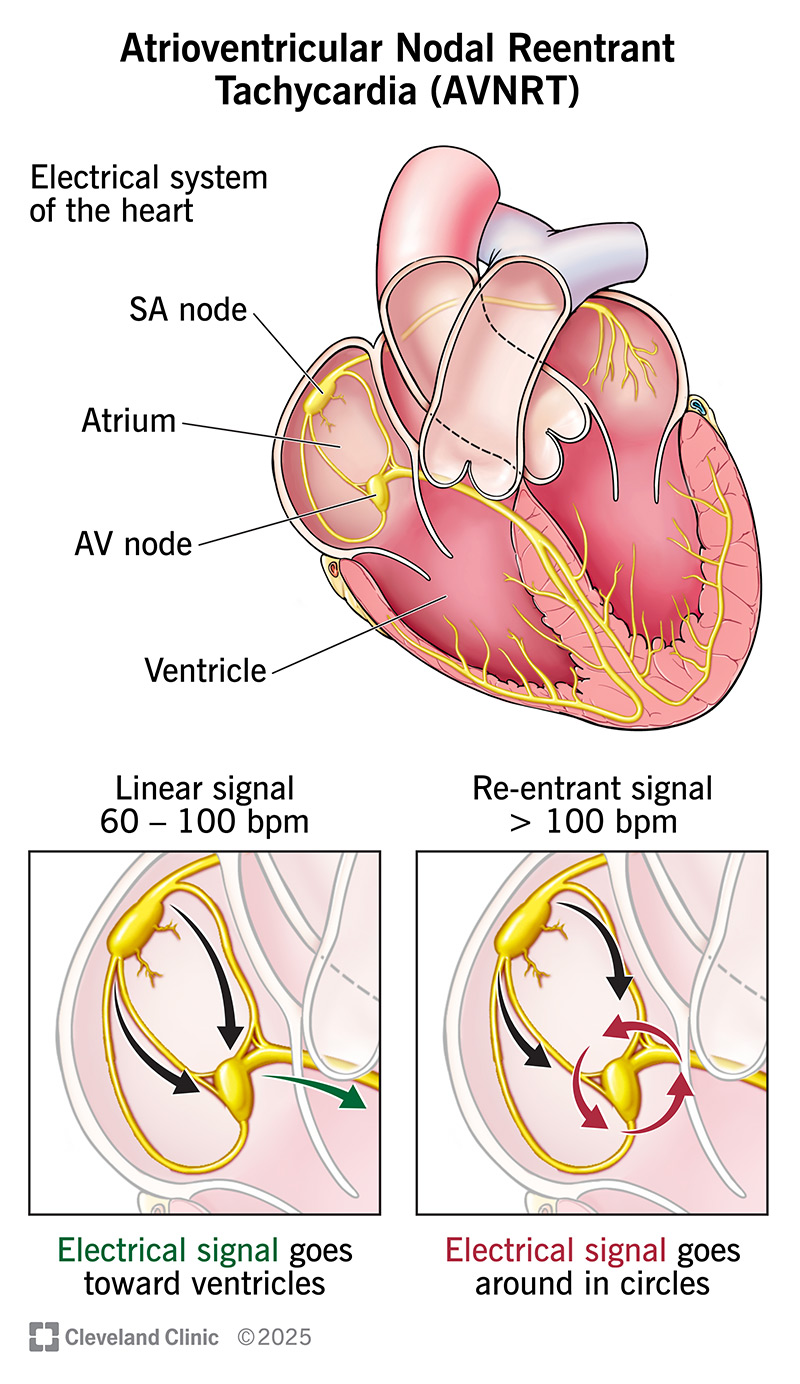
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/22923-avnrt-illustration)
This condition can make you uncomfortably aware of your heartbeat. Symptoms can include:
If you’re wearing a heart rate monitor, you might see your heart rate jump to between 120 and 200 beats per minute (bpm). This is higher than the normal adult heart rate, which is 60 to 100 bpm at rest. It’s also possible for AVNRT to make your heart rate go above 200 bpm, but this is more likely in younger people.
Advertisement
Symptoms occur in episodes that come and go. An episode might last just a few seconds or as long as several hours. Episodes start and stop suddenly.
Like other arrhythmias, this occurs when there’s abnormal electrical activity in your heart. In this case, the problem relates to your AV node.
Your AV node has a reputation for being the “gatekeeper” between your upper heart chambers (atria) and lower heart chambers (ventricles). It makes sure electrical signals get from your atria to your ventricles along a precise path.
With atrioventricular nodal reentrant tachycardia, electrical signals get caught up in your AV node. Instead of going toward your ventricles, they go around in circles in the node. When this happens, your heart can start beating very fast.
To picture this, think of cars going around and around in a traffic circle instead of exiting to a street. Normally, signals should “exit” the node and travel toward your ventricles.
It’s not always clear what triggers an episode of AVNRT. It sometimes happens on its own for no known reason. But possible triggers include alcohol, caffeine and physical activity.
Healthcare providers diagnose AVNRT by doing a physical exam and talking to you about your symptoms. They may also do one or more of the following tests:
Healthcare providers classify AVNRT into the following types:
You can’t tell which type you have based on your symptoms. But your provider can see these differences with a diagnostic electrophysiology study (EPS).
AVNRT treatment aims to manage your symptoms and improve how you feel from day to day. Unlike some other arrhythmias, AVNRT isn’t life-threatening. But episodes of a very fast heart rate can feel scary or disrupt your life.
Advertisement
Your healthcare provider will talk to you about your treatment options and help you decide what’s best for your unique needs. Certain treatments can stop an episode in its tracks. Others prevent episodes by helping your heart’s electrical system work as it should.
Treatments that can stop an episode include:
If you have frequent or severe AVNRT episodes, your provider may recommend treatments to prevent these from occurring. Such treatments help keep your heart’s electrical signals from taking the abnormal, circular route through your AV node. Options include:
Advertisement
If you’re diagnosed with AVNRT, it’s important to follow the appointment schedule your provider gives you. These give your provider a chance to check in with you about how you’re feeling.
Call your provider right away if:
AVNRT can cause uncomfortable symptoms, but it doesn’t pose a serious threat to your health. Your provider will help you understand your options for stopping episodes and, if needed, preventing future ones.
If you rarely have episodes and your symptoms are mild, your provider may recommend waiting to try treatments like cardioversion or long-term use of medicine. It’s possible you might eventually stop having any episodes even without these treatments. Your provider will help you understand what to expect in your situation.
Advertisement
It can be easy to confuse two arrhythmias that have similar-sounding names. But AVNRT isn’t the same as AVRT. The “N,” which stands for “nodal,” is important in AVNRT. It refers to the location of the abnormal electrical activity — your AV node.
AVRT is different because the problem is that there’s an extra (accessory) pathway that sends electrical signals from your atria to your ventricles. In other words, your heart has an additional wire that’s not supposed to be there and causes a fast and abnormal heart rhythm. AVRT is a feature of Wolff-Parkinson-White syndrome.
AVNRT can make both your heart and your thoughts race. While your heart is beating faster in your chest, all sorts of worries come to mind. It can be hard to tell if a fast heartbeat is harmless or something that needs medical attention.
When in doubt, listen to your body. If something feels out of the ordinary for you, call a healthcare provider. This is true whether or not you have an AVNRT diagnosis. Your provider can identify the cause and make sure you get the care you need.

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
When your heart rhythm is out of sync, the experts at Cleveland Clinic can find out why. We offer personalized care for all types of arrhythmias.
