An intrauterine device (IUD) is a form of birth control that a healthcare provider inserts into your uterus. Once it’s inserted, an IUD can prevent pregnancy for up to 10 years or more, depending on the specific type. Your provider can remove your IUD at any time if you decide to become pregnant.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
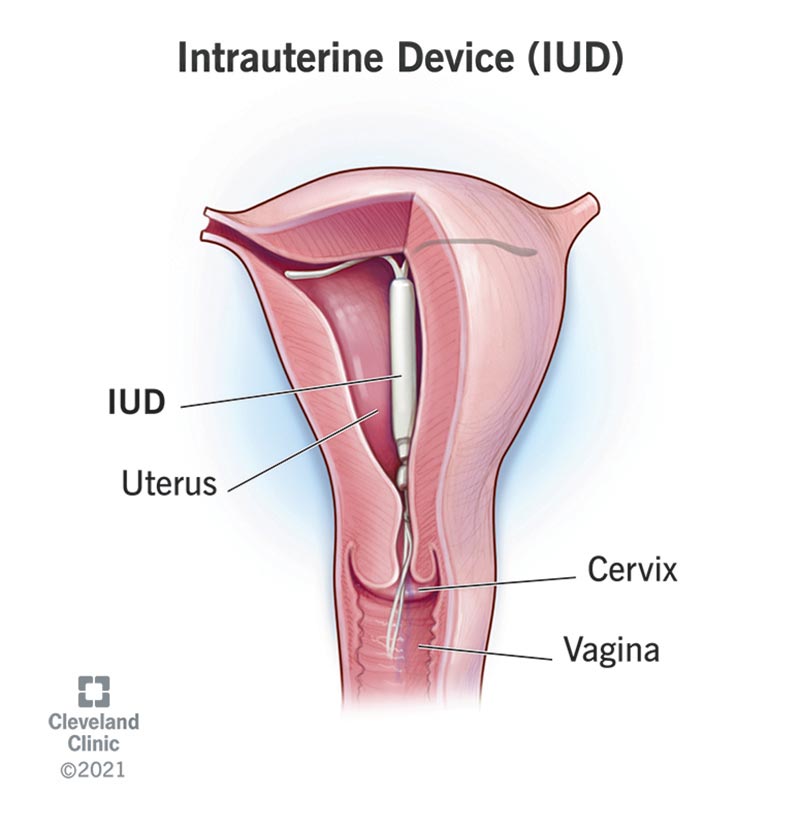
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/24441-intrauterine-device-iud)
An intrauterine device (IUD) is a type of birth control a healthcare provider inserts into your uterus. IUDs are the most commonly used type of long-acting reversible contraception (LARC). Once an IUD is inserted, you don’t have to worry about birth control until it’s time to replace it (three to 10 years, depending on the brand). LARCs, which include IUDs and contraceptive implants, are the most effective form of birth control that doesn’t require surgery.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
If you do decide to become pregnant, your provider can remove your IUD.
Unlike other forms of contraception, like condoms, IUDs don’t prevent sexually transmitted infections (STIs). You can use an IUD with condoms to prevent pregnancy while also reducing your risk of contracting an STI.
There are two kinds of IUDs, copper IUDs and hormonal (levonorgestrel) IUDs. Both have plastic frames that open into the shape of a T once inside your uterus. They have strings attached at the bottom that extend into your vagina so that your provider can remove your IUD as needed.
The FDA has approved five brands of IUDs: Paragard® (copper) and Mirena®, Liletta®, Kyleena® and Skyla® (hormonal).
Advertisement
Both types contain elements that cause them to show up during imaging procedures. Your provider can check your IUD during wellness visits to ensure it’s positioned correctly.
IUDs are the second most popular form of reversible birth control after birth control pills. Globally, around 23% of women who use contraception choose IUDs. In the United States, IUD use increased from 2% to 14% between 2002 and 2014.
You shouldn’t use an IUD if:
You shouldn’t use copper IUDs if you have a copper allergy or Wilson disease, a genetic condition that causes copper to build up in your body.
You shouldn’t use hormonal IUDs if you have severe liver disease or breast cancer. You shouldn’t use them if you’re considered high-risk for breast cancer.
All IUDs trigger an immune response. Your body recognizes an IUD as an invader and springs into action to defend itself. This process results in inflammation. Inflammation in your uterus creates an environment that’s toxic to sperm. As a result, sperm can’t reach your fallopian tubes to fertilize an egg.
The specific properties of copper and hormonal IUDs also prevent sperm from leaving your uterus.
Not all hormonal IUDs contain the same amount of levonorgestrel or have the same release rate. For example, Mirena and Liletta release more progestin than Kyleena and Skyla. Talk with your provider about which brands work best for you.
The FDA has approved the use of IUDs based on the following timeline:
Depending on factors like your age and your health, your healthcare provider may recommend that you can safely wear a device for longer and still receive the same amount of protection. Follow your provider’s guidance.
Advertisement
Only a healthcare provider can insert, adjust or remove an IUD.
Your provider will ensure you’re a good candidate for an IUD based on your health and lifestyle. You may need to take a pregnancy test or get tested for STIs beforehand.
Talk with your provider about pain management prior to your procedure. Many people tolerate having an IUD inserted with no problems. Others avoid getting an IUD because they’re concerned about what the experience will feel like. Your provider may recommend that you take pain medications beforehand to lessen any pain or discomfort you may feel. They may also numb the area before the procedure.
Communicating openly with your provider can lessen anxiety you may feel about getting an IUD.
Inserting an IUD takes fifteen minutes or less. Your provider can perform the procedure during an office visit.
You may not notice any side effects, or you may experience mild to intense pain. It’s a good idea to allow yourself some recovery time just in case. Take the rest of the day off work if you can.
Advertisement
You may:
Using over-the-counter (OTC) NSAIDs and heating pads can reduce the pain. Panty liners and pads can help manage any bleeding.
Paragard starts working immediately. Hormonal IUDs begin preventing pregnancy depending on where you are in your cycle. If you’re on your period, they start working right away. If you’re not on your period, it may take a week for them to offer you protection. Use other forms of birth control as you wait for your IUD to take effect.
IUDs are 99% effective at preventing pregnancy. IUDs and contraceptive implants are the most effective kinds of reversible birth control available.
IUDs:
Some studies have suggested that some IUD brands can reduce the risk of cervical cancer, endometrial cancer, ovarian cancer and pelvic inflammatory disease (PID).
Advertisement
Research involving Mirena and Liletta has shown that they can:
Paragard is an effective form of emergency contraception. Inserting Paragard within five days of having unprotected sex can keep you from getting pregnant.
An IUD can disrupt your menstrual cycle:
The strings from the IUD may feel stiff at first, and you or your partner may notice this during intercourse. Over time, the strings should soften. Speak to your provider if your IUD is preventing you from having a healthy sex life or causing you to experience pain during sex.
Most people who use IUDs continue to ovulate, or release an egg each month during their menstrual cycle. Ovulating may cause you to develop ovarian cysts, growths that are usually harmless and that resolve on their own. It’s common to have cysts depending on where you are in your menstrual cycle.
IUDs are considered both safe and effective. Complications — while rare — may include:
Intrauterine devices (IUDs) are a safe, effective and convenient form of birth control. Once inserted, they can prevent pregnancy for several years. Weigh the pros and cons of getting an IUD with your healthcare provider. They can help you decide if an IUD is the best option for you. They can also recommend the type of IUD that’s best for you. If you do decide to use an IUD, don’t forget to use another method to prevent STIs.

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Your birth control needs to work for you. At Cleveland Clinic, we help you find the right birth control option to fit your goals and lifestyle.
