The experience of uncontrollably leaking pee can be embarrassing for many people. Urinary incontinence is a common condition that causes you to lose bladder control. There are many different types with different causes that require unique treatment. A healthcare provider can determine the cause and recommend the right treatment for you.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
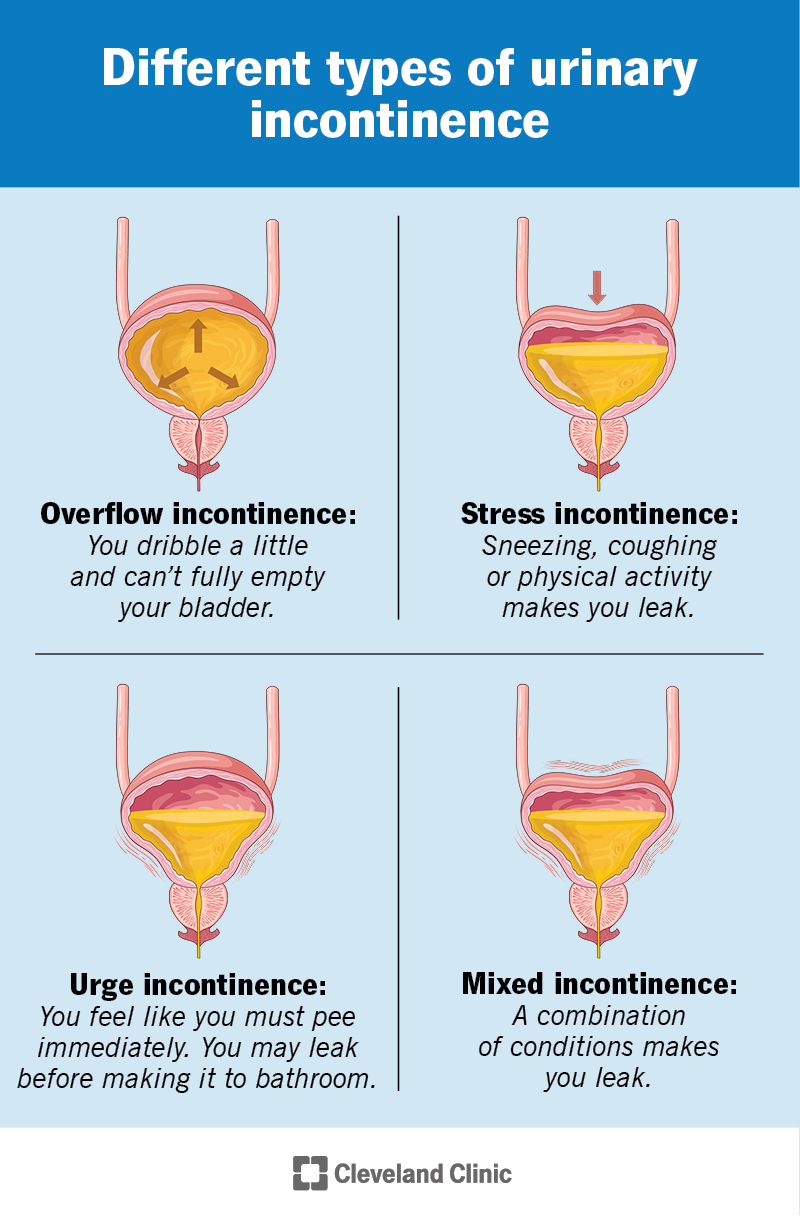
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/urinary-incontinence-v2)
Urinary incontinence is when you lose control of your bladder and leak pee. It’s a condition that can have a negative effect on your life.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Your urinary system consists of many different organs. These organs work together to filter, store and remove waste from your body as pee (urine). When your urinary system works as expected, you usually have time to get to a bathroom to pee, and you don’t leak pee. Urinary incontinence occurs when these parts don’t operate as they should. This can happen for many different reasons throughout your life.
Many people think incontinence is a normal part of getting older, and you can’t do anything to stop it. It’s true that your risk of incontinence increases as you get older. But it can happen to anyone, regardless of age. And treatments are available to help you manage it. Incontinence doesn’t have to disrupt your life or keep you from being active.
Urinary incontinence is very common. About 62% of females age 20 and older have some type of urinary incontinence. In males, a little less than 14% have incontinence.
There are many different types of incontinence. They have different causes, characteristics and triggers. Knowing the type of incontinence is an important part of your diagnosis and treatment plan.
Types of incontinence include:
Advertisement
The primary symptom of incontinence is leaking pee before you can make it to the bathroom or during activities like sneezing, coughing, laughing or exercising. If you have incontinence, you might leak a lot of pee or a small amount. It could be a constant drip or an occasional leak. Your symptoms usually depend on the type of incontinence you have. But they may include:
There are many different reasons why you might not be able to hold your pee. These may vary depending on if you’re female or male. Some causes are temporary and go away with treatment. Other causes may be chronic medical conditions. Even with treatment, chronic conditions may not go away, and you may have to manage incontinence over time as a symptom of your condition.
Temporary or short-term causes of incontinence may include:
Chronic causes of incontinence may include:
Pregnancy may cause incontinence for the following reasons:
Anyone can get incontinence. But it’s more common in certain groups of people and at certain times in your life. In females, incontinence often relates to:
Each of these can cause your pelvic floor muscles to weaken over time and make changes to your bladder that might lead to incontinence.
Yes, you’re at a higher risk of incontinence as you get older — usually over the age of 50. Your body constantly changes throughout your life.
Advertisement
Your risk for developing incontinence as you age might be higher if you:
It’s important to talk to a healthcare provider about your incontinence risks, including ways you can manage incontinence without it interfering with your daily life.
Yes, incontinence is more common in females. Pregnancy, childbirth and menopause can all lead to bladder control problems.
Pregnancy can be a short-term cause of incontinence. But bladder control issues usually get better after childbirth. Some people have experience after delivery (postpartum) because childbirth strains and weakens your pelvic floor muscles.
Menopause also causes a lot of changes in your body. Your hormones, especially estrogen, change during menopause, which can affect how you can control your bladder.
A healthcare provider can diagnose incontinence by reviewing your symptoms and medical history and performing a physical exam. They may ask you questions, such as:
Advertisement
These questions help a provider determine a pattern in your leakage, which helps them diagnose the type of incontinence. They may also perform or order tests to help them confirm the incontinence.
A healthcare provider may order the following tests to help diagnose incontinence:
Advertisement
A provider may also recommend that you keep track of any bladder leaks in a journal (bladder diary) for a few days. They may be able to identify a pattern with this information and diagnose a specific type of incontinence. Be sure to write down:
Don’t forget to bring your bladder diary with you to your appointment.
It depends. A healthcare provider must diagnose the type of continence. They’ll also talk to you about the available treatments and help you choose the one you’re most comfortable with.
The main types of urinary incontinence treatments are:
Each option has pros and cons that a provider will go over with you.
There are many urinary incontinence medications that can reduce leakage. Some drugs stabilize muscle contractions that cause an overactive bladder. Others relax muscles to allow your bladder to empty completely. If you’re in menopause, local hormone treatment, like vaginal estrogen cream, can replace the estrogen your body no longer makes and restore bladder function.
Common incontinence medications include:
Providers may start you on a low dose of medications and then increase it slowly. This helps reduce your risk of side effects and keeps track of how well the medication works.
Sometimes, changes to your everyday life can help treat incontinence without additional treatments. These changes may not be able to treat every type of incontinence. Talk to a healthcare provider before you start any of these changes.
Common lifestyle changes may include:
A provider may suggest surgery to treat your incontinence. These may include:
It depends on what type of incontinence you have. Sometimes, incontinence will go away without treatment once you address the cause, such as a UTI, certain medication or constipation.
Sometimes, urinary incontinence is a short-term issue that goes away once the cause ends, such as a UTI. But incontinence also has long-term causes. You may have incontinence for a long time, maybe even the rest of your life, if you have a chronic condition, such as diabetes or multiple sclerosis. In these cases, it’s important to talk to a healthcare provider. They can help you manage your incontinence so it doesn’t interfere with your life.
You can’t prevent all causes of the different types of incontinence. Different things in life can lead to it. But you can lower your risk by keeping your pelvic floor muscles strong with Kegels and maintaining a healthy body weight for you.
For many people, it’s helpful to talk to a therapist (counselor) or psychologist if incontinence causes stress, depression or anxiety. They can help you manage your mental health or prescribe medications.
Talk to a healthcare provider when you first notice leakage or changes to your bathroom habits. They can help determine the cause and type of incontinence and help treat or manage it.
You may want to ask your provider:
For many people, talking about their bathroom habits is embarrassing. Urinary incontinence can make you feel self-conscious or prevent you from enjoying your everyday activities because you’re worried you may leak or can’t get to a bathroom on time when the urge strikes. But a healthcare provider can help figure out the cause of your bladder control issues and help make it better. You don’t need to deal with it alone.
Talk to a provider about the best ways to treat incontinence so you don’t have to worry about leakage.

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
It can be stressful (and painful) to have bladder disorders, like urinary incontinence or cystitis. But the urology providers at Cleveland Clinic are here for you.
