An epidural hematoma (EDH) is a collection of blood that forms between your skull and the dura mater, the outermost protective membrane covering your brain. The cause is usually an artery that gets torn by a skull fracture. Symptoms include severe headache and loss of consciousness. This can be a life-threatening condition that requires emergency surgery.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
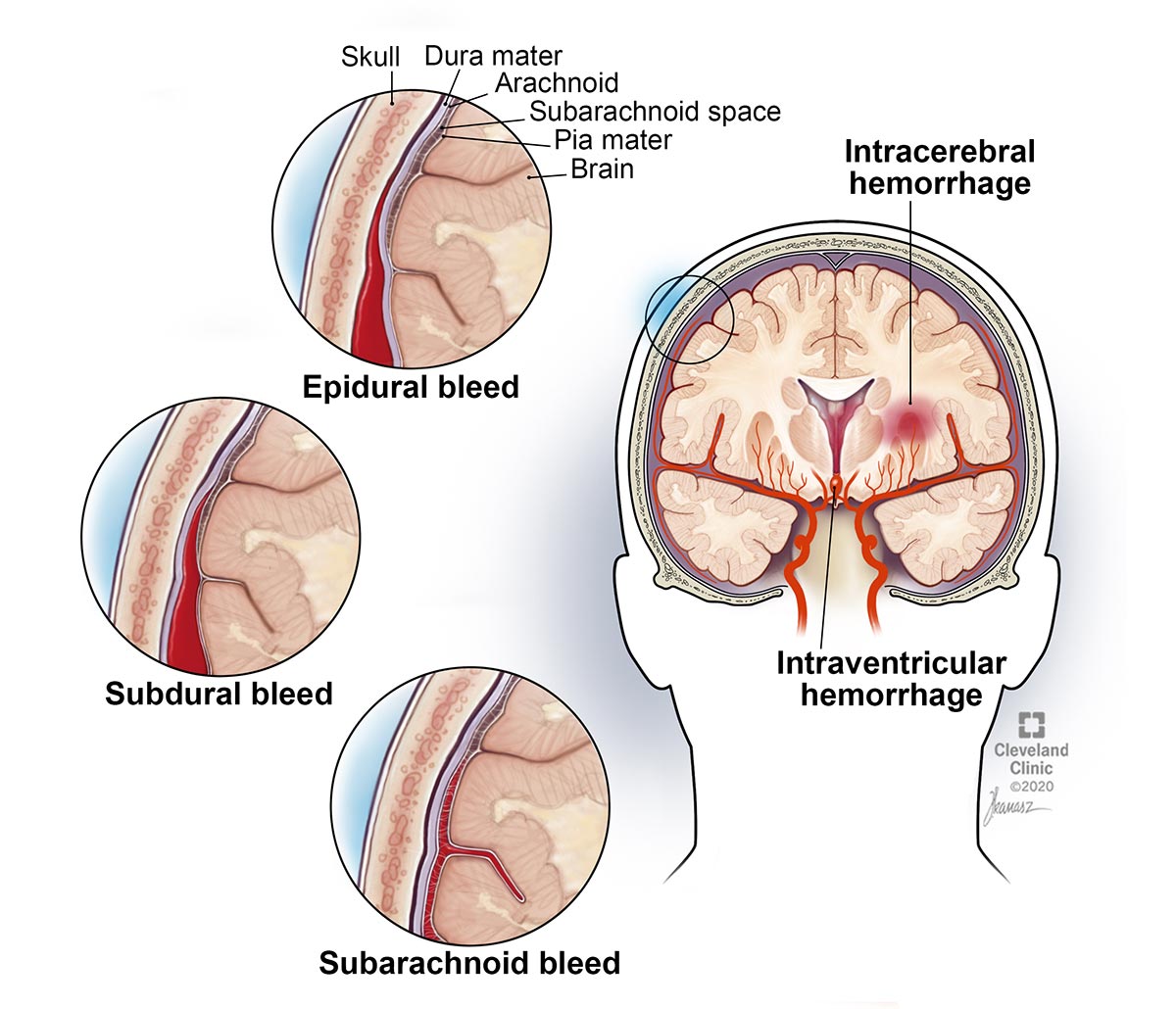
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/22034-epidural-hematoma-01)
An epidural hematoma (EDH) is a collection of blood between your skull and the dura mater, the thick membrane that covers your brain.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Your brain has three membrane layers or coverings (called meninges) that lay between your bony skull and your brain tissue. The purpose of the meninges is to cover and protect your brain and spinal cord. The dura mater is the outermost meninges.
If you have an EDH, you’ve likely had a tear in a blood vessel, usually an artery but sometimes a vein, and blood is leaking into the dura mater. The blood that leaks forms a pocket that bulges out and puts pressure on your brain. This pressure can cause more brain injury.
If bleeding occurs within the spine, it’s called a spinal EDH.
Other names for EDH are extradural hematoma, epidural hemorrhage or intracranial hematoma. More broadly, it is also a type of traumatic brain injury (TBI).
An epidural hematoma (EDH) can be a life-threatening condition. It usually requires immediate treatment or can cause brain damage or possibly death if left untreated. An EDH results in death in up to 15% of cases.
Although anyone who has a head injury can develop an epidural hematoma (EDH), they are more commonly seen in young people and specifically more often in those who have experienced a skull fracture. Typical head injuries occur during athletic activities (snowboarding, skateboarding, biking) and from car or motorcycle accidents. EDHs are four times more likely to happen in males than females. They rarely occur before two years of age or after age 60.
Advertisement
Epidural hematomas (EDHs) occur in up to 10% of people with head injuries. About 75% of EDHs in adults happen in the temporal area of the brain (side of your head over your ear).
When a person has an epidural hematoma (EDH), they experience a brief loss of consciousness after the head trauma. This is followed by a period of alertness that may last for several hours before a loss of consciousness and brain function decline. In some people, loss of consciousness leads to coma. Keep in mind that most, but not all, people with EDH follow this symptom pattern.
Other signs and symptoms of an EDH, which occur minutes to hours after the head injury, include:
If left untreated and bleeding continues, brain pressure increases and symptoms can get worse. Possible symptoms at this point include:
An epidural hematoma (EDH) is usually caused by a head injury. A skull fracture occurs in 75% of the cases. A skull fracture that tears the middle meningeal artery is the most common source of bleeding. Occasionally, an EDH can form due to bleeding from a vein.
You can also develop an EDH from non-trauma causes. These causes include:
Spinal epidural hematomas are most commonly spontaneous bleeds from veins caused by coagulopathies or over-thinning of your blood from anticoagulant medications. Other causes include:
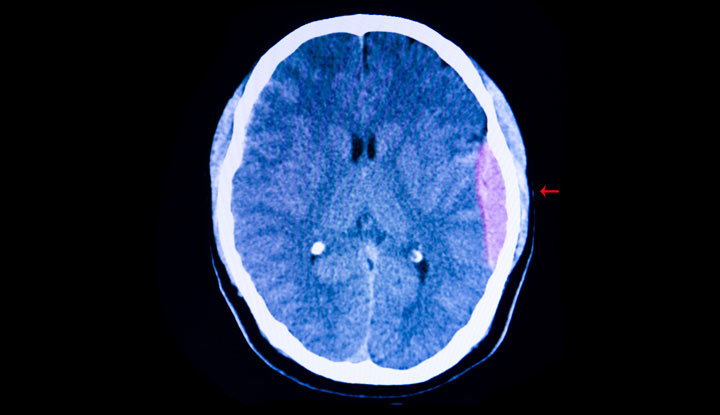
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/22034-epidural-hematoma-02)
An epidural hematoma (EDH) is diagnosed using computed tomography (CT) or magnetic resonance imaging (MRI) of your head or spine. In the head, a hematoma appears as a dense mass that pushes the brain away from the skull.
An angiogram may be ordered if a non-trauma cause, like an arteriovenous malformation, is suspected.
Blood work may be taken to look for factors that may increase your bleeding risk and check for medical problems that show your blood has problems clotting.
Epidural hematoma (EDH) usually is a medical emergency that requires immediate treatment. Signs you need surgery include:
Advertisement
Without surgery to relieve pressure on your brain, permanent brain injury or death can result.
The preferred surgery is craniotomy and hematoma evacuation. This means removing a piece of your skull and removing the blood clot, stopping any obvious sites of bleeding then putting the skull bone back in place and securing it with tiny screws.
Another surgical approach is to drill one or more holes in your skull to drain the blood. Draining the blood relieves the pressure the blood buildup causes on the brain. The drain may be left in place for several days following surgery to allow the blood to continue draining.
If you have a spinal epidural hematoma, laminectomy may be performed. During a laminectomy, a small section of bone is removed. Removing bone relieves pressure on your spinal cord and nerve roots caused by the blood clot.
Sometimes small brain bleeds that aren’t causing pressure on the brain and only cause mild symptoms can be managed without surgery. Your body can absorb a small amount of blood over time, usually a few months. If you have a small brain bleed, you’ll be closely monitored with repeat head CT scans to make sure the hematoma is healing.
Advertisement
After surgery, your neurologist or neurosurgeon may prescribe medications to reduce inflammation and pressure within your brain. Medications that may be prescribed include mannitol, hypertonic saline and glycerol. An antiseizure medication may also be prescribed for some time. Seizures are sometimes a complication of head injuries.
If you’ve experienced brain damage, your neurologist will order the needed therapy — physical therapy, occupational therapy and/or speech therapy.
Complications from surgery include:
The outcome of epidural hematoma (EDH) varies greatly from person to person. Factors that affect outcome include:
Advertisement
In general, if you have a typical EDP, your prognosis is good if the hematoma is discovered quickly and removed and you haven’t slipped into a coma. EDHs caused by a bleeding artery develop rapidly and can be found quickly. EDHs caused by a tear in a vein develop more slowly, which can delay finding and treating them. The larger the size of the hematoma, the lower the odds of a good outcome.
All blows to the head should be considered a serious event. If you or a loved one hit your head, get it checked at a hospital.
If you or someone you know has any of the following symptoms after a head injury, call 911 or seek medical attention immediately.
Although it may not be possible to prevent a hematoma as a result of a motor vehicle accident, you can reduce your risk by protecting your head when it’s an option. Always wear a helmet when riding a bike or a motorcycle or when skateboarding or snowboarding. Don’t dive into water that is not 100% free from rocks. If you play high-impact or contact sports, always wear appropriate headgear. Use safety gear if you work off the ground or at a job with a high risk of head injury. Always wear your seatbelt.
There are several differences, including:
An epidural hematoma (EDH) usually develops under a fractured area of your skull. This is a very serious, potentially life-threatening condition that requires immediate medical care. Your outcome is most promising if you are diagnosed quickly and treated. If the hematoma is large, surgery drains the blood, removes the hematoma, stops any bleeding and relieves the pressure on your brain. If the hematoma is small and you don’t have symptoms, you may not need surgery. Instead, you’ll be closely monitored with CT scans. The best advice for preventing EDHs from occurring in the first place is to wear protective headgear when work or leisure activities place your head at risk for head trauma and serious injury. Also, always wear your seatbelt in your vehicle.

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
If you have a neurological condition, you want expert advice. At Cleveland Clinic, we’ll work to create a treatment plan that’s right for you.
