An arteriovenous malformation (AVM) is a jumble of arteries and veins with no capillaries between them. This can happen in your brain or other areas. An AVM can cause bleeding or damage to tissues around it. Some people don’t have symptoms until an AVM starts to bleed. Treatments can remove an AVM, shrink it or stop blood from flowing through it.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
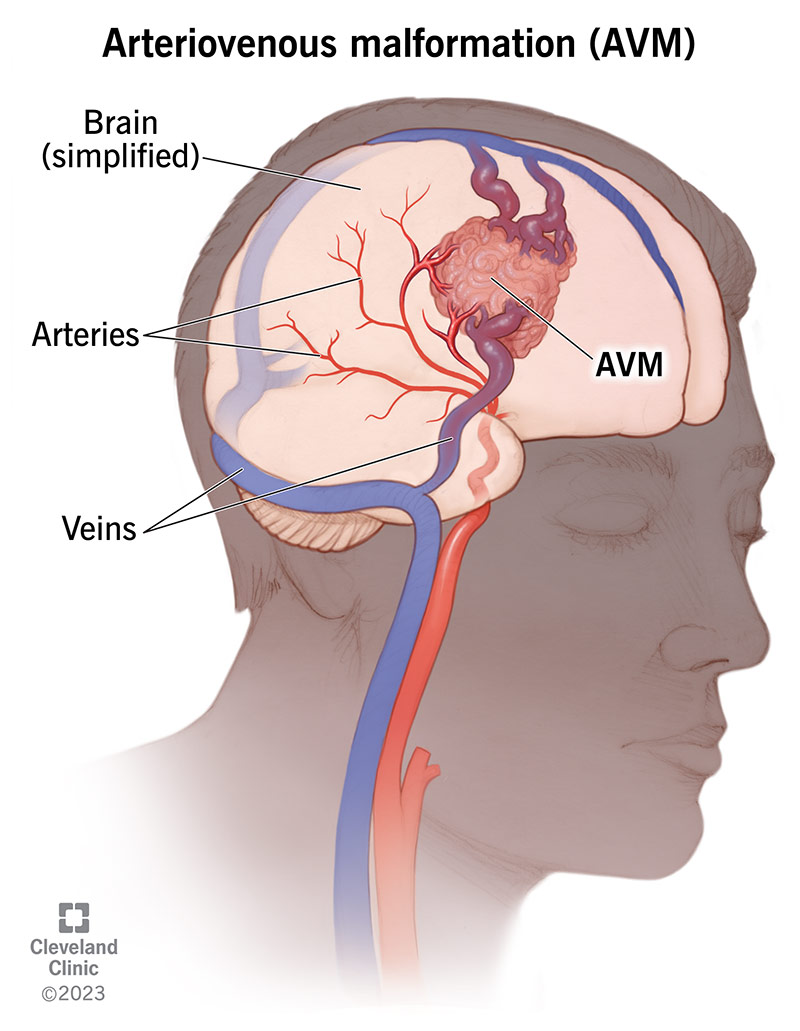
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/16755-arteriovenous-malformation-avm)
An arteriovenous malformation (AVM) is an abnormal tangle of blood vessels that looks like a bird’s nest. The tangle is made of arteries that would normally provide blood to your brain and veins that would normally drain blood from brain tissue.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Blood moves through your body within an organized closed circuit of blood vessels. Your arteries carry oxygen-rich blood from your heart to your brain and to the rest of your body’s organs and tissues. Your veins return oxygen- and nutrient-poor blood and waste products from tissues back to your heart and lungs.
Normally, the exchange takes place in your capillaries, where the smallest blood vessel units of arteries and veins connect. If you have an AVM, the “bridge” of capillaries between your arteries and veins is missing. This causes high-flow arterial blood to connect directly to veins that aren’t used to high blood pressure. As a result, the abnormal connection between the artery and vein in an AVM can cause vessel rupture and bleeding into your brain.
The two types of AVMs are:
Arteriovenous malformations are rare. They’re present in about 1 in 100,000 people. Anyone can be born with an AVM. Providers mainly discover them in people from ages 20 to 40. The risk of symptoms is highest between ages 30 and 50.
Advertisement
Arteriovenous malformation symptoms may include:
You may or may not have symptoms if you have an arteriovenous malformation. Up to 15% of people with AVMs don’t have symptoms. Often, the first sign you have an AVM is after it bleeds. If you have a brain AVM and it leads to a blood vessel bleed (rupture), it can cause a stroke and brain damage. About 50% of people with a brain AVM have a brain bleed (hemorrhage) as their initial symptom.
Scientists aren’t sure what causes arteriovenous malformations. They believe that you’re born with them and that they likely develop during fetal development (they’re congenital). AVMs may be hereditary (run in families) in rare cases.
AVMs cause harm in the following ways:
Complications of brain AVMs include:
Advertisement
Your healthcare provider will ask you about your symptoms and do a physical exam. They’ll sometimes listen for a bruit, which is a rapid blood flow sound they can hear in arteries and veins when there’s an AVM.
Imaging tests providers use to detect arteriovenous malformations include:
Brain imaging tests for suspected brain AVMs may include:
Because many AVMs don’t cause symptoms, providers only discover some of them during an imaging test for another condition (such as injuries, vision problems or headaches) or after they bleed and cause symptoms.
Advertisement
Arteriovenous malformation treatment choices depend on:
Ideally, the goal of arteriovenous malformation treatment is to reduce the chance of bleeding or make it permanently go away. There are several different ways to treat it. These treatment types include open surgery, catheter-based artery blocking, and/or focused radiation to the AVM. Any type of intervention has benefits and risks that depend your overall health and the characteristics of your AVM.
In general, treating an arteriovenous malformation as soon as possible is usually the best way to avoid serious complications.
Each person — and each person’s AVM — is unique. There aren’t any perfect decision-making tools. Your healthcare team will talk to you and your family about your situation and the best way to approach your AVM.
An AVM might be in an area where the dangers of surgery or other treatments pose a greater risk than doing nothing. If this is the case, your healthcare team may carefully monitor your AVM with imaging tests over time. If the AVM begins showing signs of change, indicating an increased risk of bleeding, your provider may consider treatment at that time.
Advertisement
Medications can relieve some of the symptoms of AVMs. These include:
Healthcare providers may try one or more of these approaches:
Complications or side effects from arteriovenous malformation treatment may include:
Each person’s AVM is a unique situation. If you’ve had surgery and a surgeon successfully removed your AVM, you’re cured of this condition.
The outcome of other AVM treatments is very good, but there are many variables, including:
Your healthcare team can best discuss your AVM and the likely expected outcome.
If you have an arteriovenous malformation and don’t get treatment, there’s a 2-4% chance per year that it’ll bleed.
No, you can’t prevent AVMs because researchers believe they’re congenital (you’re born with them). But if you develop any of the symptoms listed in this article, see your healthcare provider right away. Responding quickly to developing symptoms is the best approach.
Arteriovenous malformations can happen more than once (recur) in some people. Contact your provider if you have new symptoms. Once you’ve had treatment, you’ll need follow-up appointments with your provider every three months. After the first year, you’ll only need appointments once a year.
Get help immediately if you experience:
These are signs of a life-threatening emergency. This could be a brain bleed.
Questions to ask your provider include:
They can be. The greatest danger is bleeding (hemorrhage). If you feel a sudden, severe headache (“worst in your life”), call 911. You might have a bleeding brain AVM. There’s a 2-4% chance of bleeding per year with for unruptured AVMs. Seventeen percent of previously ruptured AVMs burst (rupture) every year.
No. Some arteriovenous malformations never cause a bleed and may not even cause symptoms or any health problems your entire life. Healthcare providers only discover some AVMs during an imaging test for another reason or during an autopsy after death.
AVMs can cause health issues other than bleeds. Some AVMs that grow and become large can press on an area of tissue and cause tissue damage, nerve cell damage and other cell damage in that area. If large enough and in a vital area, the lack of capillaries between your arteries and veins can cause a lack of oxygen, nutrients and waste exchange in tissue in this area. This can lead to tissue death.
Yes, they can be. How deadly or severe an arteriovenous malformation might be depends on its size and location. A massive bleed from a ruptured AVM in your brain can be fatal. However, some people have AVMs and never have any symptoms or health problems.
Not necessarily. It may, but most often, the location you feel headache pain isn’t specific to the area of the AVM.
In some people, the changes pregnancy brings can cause AVM symptoms to appear suddenly or get worse. The increase in blood volume and blood pressure that comes with pregnancy can increase the risk of an AVM bleed.
AVMs can cause behavioral changes or small changes in your child’s ability to learn. These changes might happen before more obvious symptoms develop when your child is older (if symptoms develop).
No. Some very small brain bleeds, called microbleeds, cause limited damage and few symptoms. But over time, many microbleeds can increase the risk of dementia and impair thinking functions.
An aneurysm is a weakened, ballooned-out area in an artery. It most commonly forms at the point where two arteries branch. An aneurysm can develop as a complication of an AVM.
Hemangiomas are vascular (blood vessel) malformations you can see on your skin. They aren’t dangerous and don’t require treatment.
Cavernous malformations are a type of vascular lesion. Unlike an AVM, they contain slow-moving blood that’s usually clotted. They can leak but usually don’t bleed as severely as AVMs and often don’t cause symptoms.
A fistula is a general term for an abnormal connection of blood vessels. Arteriovenous fistulas can happen in the tissue that covers your brain and spinal cord. AVMs can happen inside your brain’s tissues. Fistulas are more commonly associated with head trauma or infection than AVMs.
An arteriovenous malformation (AVM) is a serious medical condition, but available treatments are highly effective. Your healthcare team will talk with you about the details of your AVM — its size and location — and other factors to develop treatment options that are best for you. Don’t be afraid to ask questions if anything isn’t clear. You owe it to yourself to understand your options.

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
If you have a possible arteriovenous malformation (AVM), you’ll want experts by your side. Cleveland Clinic’s providers are here to get you the care you need.
