A subdural hematoma is a type of bleeding near your brain that can happen after a head injury. Symptoms like a headache and slurred speech can develop right after the injury or days to months later. Subdural hematomas can be life-threatening, so it’s crucial to see a healthcare provider whenever you have a head injury.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
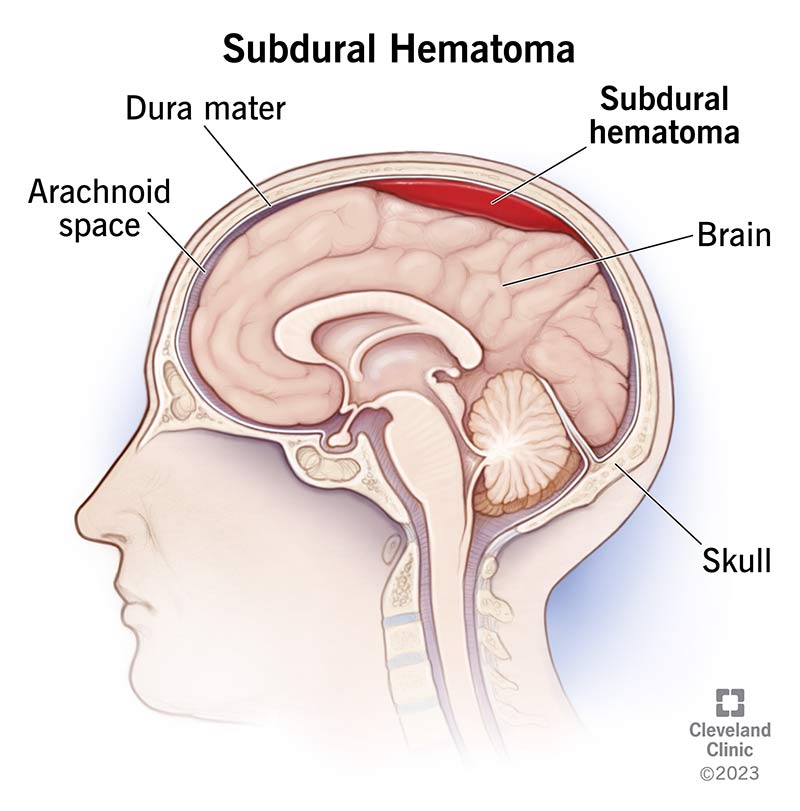
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/21183-subdural-hematoma)
A subdural hematoma is a type of bleeding inside your head. It happens when blood collects under the dura mater, one of the layers of tissue that protect your brain. It most often happens from a head injury and can be fatal.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
The dura mater is one of the meninges — the three layers of membranes that cover and protect your brain and spinal cord. They include:
A subdural hematoma develops from a tear in a blood vessel. Blood leaks out of the torn vessel into the space between your dura mater and your arachnoid mater. Active bleeding into this space is called a subdural hemorrhage. A buildup of blood is a subdural hematoma.
More broadly, a subdural hematoma is a type of traumatic brain injury (TBI).
Subdural hematomas can be life-threatening and need immediate medical care.
Healthcare providers sort subdural hematomas by:
The types of subdural hematomas include:
Advertisement
Subdural hematomas happen in around 1 in 4 people with head injuries.
Symptoms of a subdural hematoma may appear immediately following trauma to your head. Or they may develop over time — even weeks to months after the injury.
Signs and symptoms of a subdural hematoma include:
Symptoms of chronic subdural hematoma may also include:
A baby with a subdural hematoma may have an enlarged head. This is because their soft skull can enlarge as blood collects.
Get immediate medical help if you or a loved one have these symptoms.
As bleeding continues and the pressure in your brain increases, symptoms can get worse. Severe symptoms include:
Sometimes, people have no symptoms immediately following a head injury. This is called a lucid interval. They develop symptoms days later. Also, it’s important to know that subdural hematomas that develop more slowly (the chronic type) might be mistaken for other conditions, such as a brain tumor, stroke or dementia.
Any time you experience neurological symptoms, like memory loss, dizziness or muscle weakness, you should see a healthcare provider. Try to give them as much information as possible about when and how your symptoms started.
Head injuries cause most subdural hematomas. Examples of how this could happen include:
Anyone can get a subdural hematoma from an accidental head injury. But certain factors can increase your risk, including:
Advertisement
A healthcare provider will do a thorough physical and neurological exam. They’ll ask about:
If the provider thinks you may have a subdural hematoma, they’ll order an imaging test of your head. This may be a computed tomography (CT) scan and/or a magnetic resonance imaging (MRI) scan. These tests allow providers to see clear pictures of your brain and determine the location and amount of bleeding. They can also show other head and neck injuries.
In an emergency, healthcare providers will stabilize your breathing and other vital signs.
For large or severe subdural hematomas, you usually need surgery. There are two main types:
Advertisement
Sometimes, hematomas cause few or no symptoms and are small enough that they don’t require surgical treatment. Rest, medications and observation may be all that you need. Your healthcare provider may order regular imaging tests (such as an MRI) to monitor the hematoma and make sure it’s healing.
Like all surgeries, craniotomies and burr hole surgeries carry a risk of complications. Most of these complications are uncommon, but they can be serious.
Problems that can develop after subdural hematoma surgery include:
The length of time it takes to recover from a subdural hematoma varies from person to person. Your healthcare provider can tell you what to expect based on your unique situation. Some people feel better a few weeks after treatment, while others may never make a full recovery.
If you have persistent symptoms after surgery like memory problems or weakness, you may need further treatment to help you gradually return to your normal activities.
You may have several healthcare providers as a part of your rehabilitation, including:
Advertisement
If you have a subdural hematoma, your prognosis (outlook) depends on:
About half of people with large acute hematomas survive, but they often have permanent brain damage. Younger people have a higher chance of survival than older adults.
In some cases, the hematoma can come back during the days or weeks after surgery. If this happens, you may need another surgery.
People with chronic subdural hematomas usually have the best prognosis, especially if they have few or no symptoms and remained awake and alert after the head injury.
Without treatment, large hematomas can lead to coma and death. Other complications include:
Children with severe hematomas may have developmental delays from permanent brain damage.
Subdural hematomas can be life-threatening. If you have a head injury, get immediate medical attention. Don’t wait to see if symptoms develop. It’s better to know right away. If you’re at risk of subdural hematomas based on your age, medications you take or health conditions you have, talk to your healthcare provider about ways to lower your risk. They’re available to help.

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
If you have a neurological condition, you want expert advice. At Cleveland Clinic, we’ll work to create a treatment plan that’s right for you.
