Transient ischemic attacks (TIAs) are often incorrectly called “mini-strokes,” but they’re every bit as serious as a true stroke. Having a TIA often means you could have a stroke in the very near future. A TIA is a medical emergency you shouldn’t ignore. More importantly, it’s a chance to get treatment that can prevent a future stroke.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
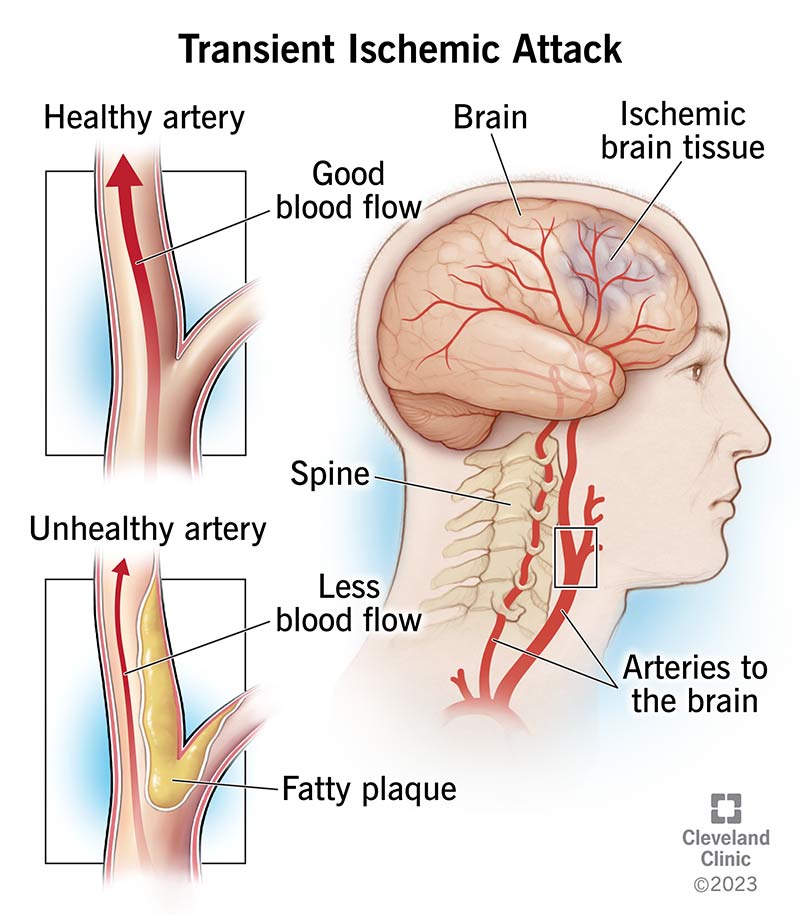
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/14173-transient-ischemic-attack)
A transient ischemic attack is like a temporary stroke. It means there’s a temporary (transient) lack of blood flow to part of your brain. Without blood flow, the brain cells malfunction and start to die (ischemia).
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Often shortened to TIA, a transient ischemic attack is a medical emergency that’s very similar to an ischemic stroke. The symptoms of the two are the same, but TIA symptoms go away within 24 hours (most go away in minutes).
IMPORTANT: A transient ischemic attack is a medical emergency just like a stroke is. That’s because there’s no way to predict how long a TIA will last, and every minute counts. Seek immediate medical help if you have signs of stroke, including balance issues, vision changes, face and arm drooping, and speech difficulties.
If you or someone you’re with has TIA or stroke symptoms, you should immediately call 911 (or the local emergency services number in your area). Don’t wait to see if the symptoms will subside, and don't avoid calling if the symptoms get better after a few minutes of resting. A TIA can be the precursor to a stroke, so get medical attention right away!
A common nickname for TIAs is “mini-strokes.” But that’s not an accurate name. A TIA isn’t necessarily “mini” or smaller, and TIAs can easily affect large brain areas. Importantly, a stroke may occur after a TIA, within a matter of minutes, hours or days.
There are also two critical differences between strokes and TIAs. The first is that a TIA stops on its own. A stroke doesn’t, and it needs treatment to stop and reverse the effects. A stroke also leaves behind evidence on a magnetic resonance imaging (MRI) scan. The changes remain even if your symptoms go away.
Advertisement
The possible symptoms of a TIA are nearly identical to the possible symptoms of a stroke.
The symptoms of an ischemic stroke can involve one or more of the following:
Transient ischemic attacks and ischemic strokes happen for the same reasons. Those reasons include:
Many factors can contribute to a TIA or make one more likely to happen. Risk factors include:
Other risk factors that can contribute to a TIA include:
The main reason that a TIA is a medical emergency is because it’s often a warning that a stroke is possible or even imminent. Up to 20% of people who have a TIA have a stroke within 90 days, and half of those strokes happen within the first two days after a TIA.
Advertisement
A healthcare provider can diagnose a TIA using a combination of methods, including:
Other tests may also be possible, depending on your symptoms and if your healthcare provider suspects another health issue is causing or contributing to the TIA and its symptoms. Your healthcare provider can tell you more about the tests they recommend and why those tests could be helpful.
A TIA, by definition, is a temporary issue. But it indicates that a stroke — which isn’t temporary — could happen. That means treating the condition(s) that caused the TIA can help prevent a stroke.
Healthcare providers often recommend treating these conditions aggressively. That’s because a stroke is a much more serious — and dangerous — condition. Strokes are also often more difficult to treat. It’s also because even with treatment, strokes can cause permanent damage or death.
Advertisement
The most common treatments to prevent a stroke after a TIA include:
Many types of medications can help treat the conditions that cause or contribute to a TIA and prevent TIA or stroke from happening in the future. They include:
Advertisement
“Endovascular procedures” is the blanket term for all procedures that use thin, tube-like devices threaded into your blood vessels through very small incisions in your skin. Endovascular means “inside a blood vessel,” and these procedures treat problems from the inside without full surgery.
These usually involve your carotid arteries, the main vessels that carry blood from your heart to your brain. Narrowing (stenosis) in your carotid arteries can lead to a TIA or a stroke.
Some examples of endovascular procedures that can help prevent a stroke after a TIA include:
When catheter-based procedures aren’t possible, surgery may be an option to widen blood vessels. That can prevent another TIA or stroke. An example of a surgery like this is carotid endarterectomy to clean up the plaque and create a wider space for blood to flow through into your brain.
Other procedures are also possible, depending on what conditions you have. For example, your cardiovascular or cerebrovascular care team may determine that your TIA or stroke is due to conditions like patent foramen ovale (PFO), a hole in the wall that separates the upper two chambers of your heart. PFO can allow blood clots to travel to your brain. Your provider may recommend closing the hole to reduce the odds of having a stroke.
Having a TIA is like having a temporary stroke. If they happen while you’re active, the symptoms may stop or lessen if you rest because you don’t feel well. However, the symptoms can return quickly once you resume whatever you were doing.
Because a TIA and a stroke have the same possible symptoms, you should always call 911 (or your local emergency services number) immediately. There’s no way to tell if what you’re experiencing is a stroke or a TIA while it’s happening.
How long TIAs last can vary. By definition, TIAs last less than 24 hours. But it’s rare for a TIA to last even that long. Most TIAs last for only minutes.
The outlook for a TIA depends strongly on what’s causing it and what you do about it. Without treatment, your stroke risk within the next 90 days — especially the first two days after the TIA — can be very high.
The outlook is best when you get immediate emergency medical care. Healthcare providers can make sure that what you had was a TIA and not a stroke, and they can find out what’s causing or contributing to your TIA. That can also determine how to treat the underlying issue and what you can do to prevent further issues.
Sometimes, but not always. Many TIAs happen for preventable reasons. But a TIA can also happen for unpredictable or unexpected reasons.
You can do many things to reduce your risk of having an ischemic stroke. While this doesn’t mean you can prevent a stroke, it can lower your risk. Actions you can take include:
Once you receive care, it’s essential for you to follow your healthcare provider’s guidance. The closer you follow it, the better the odds that you won’t have another TIA or stroke. Because TIAs can happen for different reasons, what you should do to take care of yourself may vary.
In general, the same actions or precautions that prevent TIAs or lower your risk of having one are also what you should do after you have a TIA. Your healthcare provider can also guide you specifically on what you can and should do.
After emergency treatment for a TIA, you should see a provider for follow-up care. They can recommend a schedule for follow-up visits as needed and help you monitor for any changes in symptoms and how well treatment is working.
You should immediately call 911 (or your local emergency services number) and go to the nearest emergency room if you have any stroke-like symptoms. If you previously had a TIA, you should call 911 (or your local emergency number) and go to the nearest ER if any of the symptoms return.
Several other conditions are possible if you recently had a TIA. You should get emergency care if you experience symptoms of any of the following conditions:
TIAs are very common. Experts estimate there are about 500,000 per year. However, there’s evidence that estimate is too low. The reasons for that include:
A transient ischemic attack (TIA) can happen suddenly and be gone in minutes, leaving behind confusion and worry. If you experience stroke symptoms that only last minutes, don’t ignore them! They’re still a sign that you need medical attention right away.
A TIA greatly increases your risk of having a stroke in the next 90 days, and half of the strokes that do follow a TIA happen within the next two days. Getting immediate care can help you avoid a much more serious stroke, potentially saving your life and preventing permanent damage and loss of abilities.
Learn more about the Health Library and our editorial process.
Cleveland Clinic's health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability, and up-to-date clinical standards.
Cleveland Clinic's health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability, and up-to-date clinical standards.
After a stroke, it’s essential to get treated right away. Cleveland Clinic’s stroke care specialists can help you manage recovery and improve your quality of life.
