Carotid artery stenting is a minimally invasive procedure to treat carotid artery stenosis and prevent stroke. A stent in your carotid artery increases blood flow to your brain. Carotid artery stenting has some advantages over a more invasive procedure, but it also has risks.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
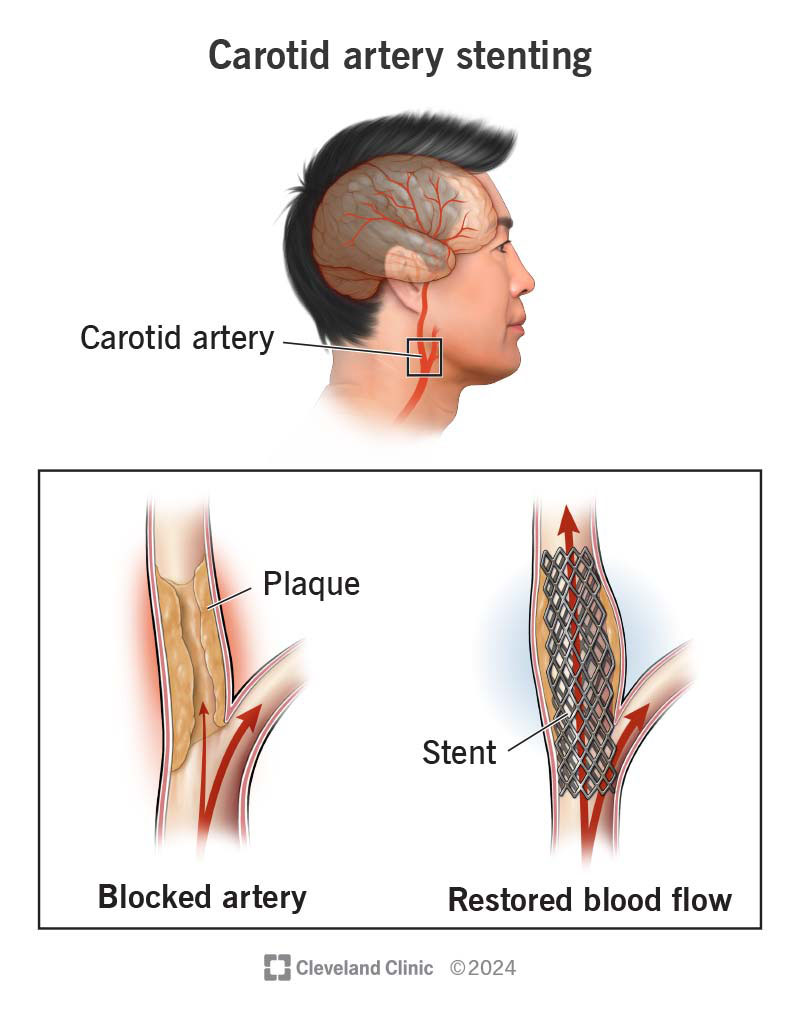
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/16850-carotid-artery-stenting)
Carotid artery stenting is a procedure to prevent a stroke. A healthcare provider can perform this procedure if a carotid ultrasound, CT scan or MRI shows you have a blockage in your carotid artery. Your carotid arteries are blood vessels that supply blood to your brain, face and neck. Sometimes, a fatty material (plaque) builds up in your arteries and causes a blockage.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
A healthcare provider can put in a stent (a small, metal mesh tube) to open the blockage. Putting a stent in your carotid artery keeps it open to allow better blood flow to your brain. This lowers your risk of a stroke.
The stent stays in place permanently. It acts as a scaffold to support the artery and keep it open. After several weeks, the carotid artery heals around the stent.
Depending on what part of your carotid artery has the blockage, a provider will use a specially designed stent that is specifically approved for this purpose. The place where your carotid artery branches to supply your face and brain is the most common place for a blockage to happen.
A specially trained provider performs carotid artery stenting. This can be an interventional cardiologist, vascular surgeon, endovascular neurosurgeon, interventional neuroradiologist or neurologist. They can access your carotid artery by way of an artery in your leg or arm or through your neck (where your carotid artery is). Your provider can tell you which method is best for you.
A carotid artery stenting procedure treats carotid artery stenosis (narrowing). The U.S. Food and Drug Administration (FDA) approved carotid artery stents beginning in 2004. People who get this procedure usually have:
Advertisement
You may need to take aspirin and a second antiplatelet medicine (like clopidogrel, ticagrelor or prasugrel) for three to five days before your carotid artery stenting procedure and continue after the procedure. Failure to take these medicines will require a delay in performing your procedure. Your provider will give you specific instructions about what you can and can’t eat or drink before the procedure, too.
Your healthcare provider may perform one of two types of carotid artery stenting:
The type determines how they’ll access your carotid artery. The procedures are somewhat similar except for the access point and the way they deal with plaque particles. Your provider will choose the best option for you.
Access points for each procedure are:
During the procedure, you’ll receive medication like heparin or bivalirudin to reduce the risk of blood clots. You’ll need to keep the site of entry (leg or arm) straight and still for two to six hours after the procedure.
A carotid artery stenting procedure usually takes about one to two hours. However, the preparation and recovery time add several hours. You can expect to stay at the hospital all day for the procedure and will stay overnight.
After a provider places the carotid artery stent, they’ll:
Follow your healthcare provider’s instructions about how and when to take these medications. Don’t stop taking them without first talking to your provider. They’ll determine how long you’ll need to take these medications, but it will be at least one month. But in many cases, it’s at least six months.
Advertisement
People who have carotid artery stenting instead of a carotid endarterectomy have these benefits:
For most people, carotid artery stents increase blood flow to their brains and decrease their risk of a stroke.
Researchers have compared the results of the carotid stenting procedure with that of the carotid endarterectomy surgery. Studies have found that there were no significant differences in major risks of the two treatments through 10 years.
However, people who get a stent in their carotid artery may be more likely to have a minor stroke. But they also don’t have the risks of nerve damage.
Both treatments have similar rates of restenosis (an artery getting narrow again). This can happen in the first two years due to scar tissue or later from the process of atherosclerosis or hardening of the arteries. Both treatments have a likelihood of being a lifetime repair in over 95% of cases.
Although the carotid stenting procedure opens up a blocked carotid artery, it doesn’t cure carotid artery disease. You’ll still need to focus on reducing your risk factors and making certain lifestyle changes to prevent atherosclerosis from developing or getting worse.
Advertisement
For the best results, follow these recommendations:
Some of the possible carotid artery stenting risks include:
There may be other possible carotid artery stenting complications. When you meet with your healthcare provider, ask questions to make sure you understand the potential risks and benefits of the procedure. Certain risk factors may make you ineligible for carotid artery stenting.
Carotid artery stenting risks vary depending on:
You’ll need to take it easy for a few days after the carotid artery stenting procedure.
Advertisement
Follow these guidelines:
If you have bruising in your groin, arm or neck area, it should go away in a week or less.
It’s important to call 911 or emergency services if you have stroke symptoms similar to what you experienced before your carotid artery stenting procedure. This includes facial asymmetry, any speech issues (like an inability to talk), or an inability to move or feel parts of your body.
If you have any bleeding or drainage from the puncture site, call your provider as soon as possible.
Scar tissue at the treatment site can cause another blockage, or restenosis. This re-narrowing in the treated carotid artery is more likely to occur in the first 24 months after treatment. Providers check for this with a carotid ultrasound. This is why keeping your follow-up appointments is important. Various studies estimate the rate of restenosis at 11% to 40%. However, significant narrowing requiring retreatment occurs in less than 5% of cases.
Talk with your provider about which treatment for carotid artery stenosis is best for you. Carotid artery stenting is a good option for some people, but a different procedure may be better for others. If you end up having a carotid artery stenting procedure, using a facility that does a lot of them can give you peace of mind. It’s important that the provider doing the procedure has performed them many times. Don’t be afraid to ask your doctor questions about their experience and your concerns.

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
When the carotid arteries in your neck are blocked, you’re at risk for a stroke. Cleveland Clinic’s experts are world renowned in treating this condition.
