Colon polyps are growths, like tiny bumps, that form on the inside lining of your colon or rectum. They’re usually harmless, but some types can turn into colon cancer after many years. Healthcare providers remove colon polyps when they find them during a routine colonoscopy.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
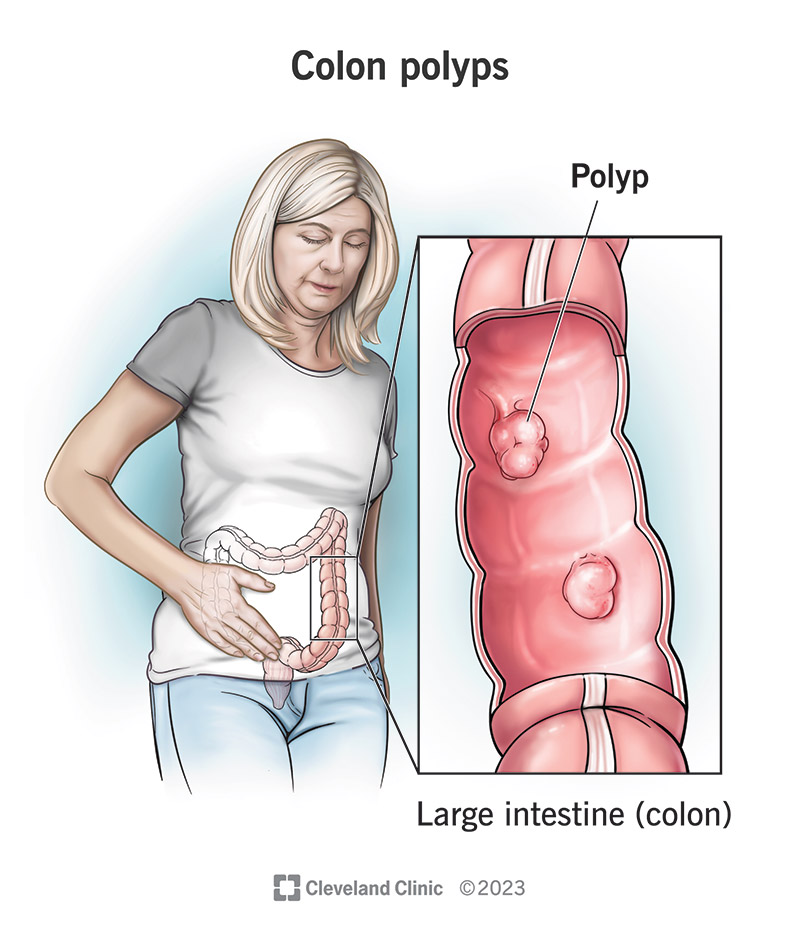
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/Images/org/health/articles/15370-colon-polyps)
Colon polyps are growths on the inside lining of your colon (large intestine). They’re a type of tumor, a cluster or mass of abnormal cells. Polyps are tumors that grow out of the mucous lining inside your hollow organs, like your gastrointestinal tract, your nose or female reproductive organs.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Colon polyps are common, and many are harmless. But some types can grow into cancer if they aren’t removed. This is why healthcare providers look for polyps in your colon during a colonoscopy, an exam inside your colon. While polyps aren’t cancer, almost all colorectal cancer starts from a polyp.
Healthcare providers classify colon polyps in a couple of different ways. One way is by looking at the shape. If a polyp looks like a mushroom, with a “head” and “stalk,” they call it “pedunculated.” If it doesn’t have a stalk and looks more like a raised lump with a broad base, they call it “sessile.”
Providers also consider how polyps look under a microscope. Different types have different microscopic features because they grow and develop using different processes. These same processes also determine whether a polyp can grow into cancer or not. So, different types have different cancerous potential.
Types of colon polyps include:
Healthcare providers classify colon polyps as neoplastic or non-neoplastic to indicate whether they can grow into cancer or not. Neoplastic polyps can grow into cancer. Non-neoplastic polyps can’t.
Advertisement
Neoplastic polyps include:
Non-neoplastic polyps include:
Colon polyps are common, especially as you get older. They affect about 20% of adults overall and about 40% over the age of 50, as well as 6% of children. Everyone is at risk for colon polyps and colon cancer, regardless of sex or where your family is from. But, in general, they’re slightly more common in Western nations.
Most colon polyps have the potential to become cancerous, which is why healthcare providers remove them during a colonoscopy. But very few of them actually do turn into cancer, and it takes a long time for them to do so. Routine colonoscopies remove polyps before they have the chance to become cancer.
Around 75% of colorectal cancers start from adenomatous polyps, and about 80% of all colon polyps are adenomas. But only about 5% of adenomas are actually malignant. The risk of a random, average-size colon polyp becoming cancerous is estimated to be 8% over 10 years and 24% over 20 years.
Most colon polyps, and many colorectal cancers, won’t cause any symptoms. This is why screening — testing for diseases before you have symptoms — is so important. Usually, by the time you do have symptoms, the polyp has already turned into cancer.
Possible symptoms, though uncommon, include:
Most colon polyps are sporadic, which means they occur randomly. However, some people have hereditary syndromes, conditions passed down through their families, that cause colon polyps. These syndromes can cause large numbers of certain types of polyps and can carry a higher cancer risk.
Genetic mutations are the main cause of colon polyps. These are errors in the genetic code that your cells use to reproduce themselves. The cells in your colon lining replace themselves often, so there are more chances for errors to occur. When their code changes, they grow and behave differently.
Some gene mutations are passed down through families (these are hereditary syndromes). Others appear to be random, but they probably have multiple contributing causes. Researchers believe that sporadic colon polyps may be partly inherited and partly triggered by environmental risk factors.
Advertisement
Genetics: You’re more likely to have sporadic colon polyps if you have a first-degree relative who’s had them. You may also have colon polyps associated with a specific hereditary syndrome.
Genetic disorders that cause colon polyps include:
Environment: Environmental risk factors are factors related to where and how you live that can affect your colon health. They include your physical environment, social environment and lifestyle habits.
Environmental risk factors that may contribute to colon polyps include:
Exceptions: Inflammatory pseudopolyps aren’t true polyps and aren’t caused by genetic mutations. They’re ulcers that healed to form bump-like scars that look like polyps. Chronic inflammation in your colon (colitis) is the usual cause of these ulcers. They’re often related to inflammatory bowel disease (IBD).
The best way to find and identify colon polyps is with a colonoscopy. This is an exam that looks inside your colon with a lighted camera. While other types of imaging tests can find colon polyps, a colonoscopy allows a healthcare provider to find and remove polyps during the same procedure.
Advertisement
Your healthcare provider can pass tools through the colonoscope to remove polyps or take tissue samples during your colonoscopy. They send these samples to a lab for further study. A pathologist examines the polyp samples under a microscope to identify the type and check for cancer cells.
A colonoscopy does involve some preparation and the use of anesthesia, which may be difficult for some people. Healthcare providers may begin with simpler screening tests for these reasons. However, if another test did find colon polyps, you’d still need to have a colonoscopy to remove them.
Additional tests that may suggest colon polyps include:
Advertisement
It’s normal to have anywhere from no colon polyps to a few. Healthcare providers pay attention to the number of polyps you have, as well as their size, location and type. Since polyps grow very slowly, having fewer and smaller polyps means you’re still at a relatively low risk of developing colorectal cancer.
You may be at a higher risk of developing colon cancer if you have:
The standard treatment is to remove colon polyps, unless you only have non-neoplastic types. Sometimes, a pathologist must examine them under a microscope before identifying them as neoplastic or non-neoplastic. It may take a week or two for your biopsy results and diagnosis to come back to you.
Removing neoplastic polyps reduces your risk of developing colorectal cancer by 80%. But once you’ve had polyps, you’re likely to have them again. Your healthcare provider will judge your risk of future polyps based on the polyps you’ve had before. They’ll schedule your next screening based on that risk.
Healthcare providers who conduct colonoscopies — usually, a gastroenterologist or colorectal surgeon — can remove most of your colon polyps during your screening. This simple procedure is called polypectomy. Occasionally, some polyps require special procedures to remove them (EMR or ESD).
If your colonoscopy doesn’t find any neoplastic polyps, you may not need another one for 10 years. But if you do have neoplastic polyps removed, this may change when you need to have your next screening. Your provider will recommend you come back in one, three, five, or seven years, depending on your personal risk factors.
Colon polyps can be serious because of their potential to turn into cancer. But most polyps aren’t cancerous when they’re found. Some might grow into cancer over time if they’re left untreated. Healthcare providers remove them when they find them to prevent this from happening.
There’s no way to prevent the genetic mutations that result in colon polyps. But you may be able to reduce your risk by taking good care of your general health. Eating more whole foods and fewer animal fats, getting some exercise and avoiding heavy drinking and smoking can help prevent colorectal cancer.
You might want to ask:
Many people dread their routine colonoscopy screening and wonder if they can put it off. It might seem like a lot of trouble to go through just to confirm that you don’t have colon polyps. But if you do, a colonoscopy is your best chance of having them diagnosed and treated before you even know it.
It might be scary to learn that you have colon polyps, but many people do, and most will never get cancer. A colon polyp that’s been found and removed is one that you don’t have to worry about. The important thing is that it’s found and removed early enough to prevent cancer from starting.
Learn more about the Health Library and our editorial process.
Cleveland Clinic's health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability, and up-to-date clinical standards.
Cleveland Clinic's health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability, and up-to-date clinical standards.
A colonoscopy or other screening is an important test for colon cancer. The team at Cleveland Clinic can give you peace of mind and expert care when you need it.
