Ischemic colitis is one of many types of colitis, which means inflammation in your colon. But unlike other types, ischemic colitis begins in your circulatory system. Reduced blood flow to your colon deprives the tissues of oxygen, causing an inflammatory response. If blood flow isn’t restored, it could cause tissue death.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
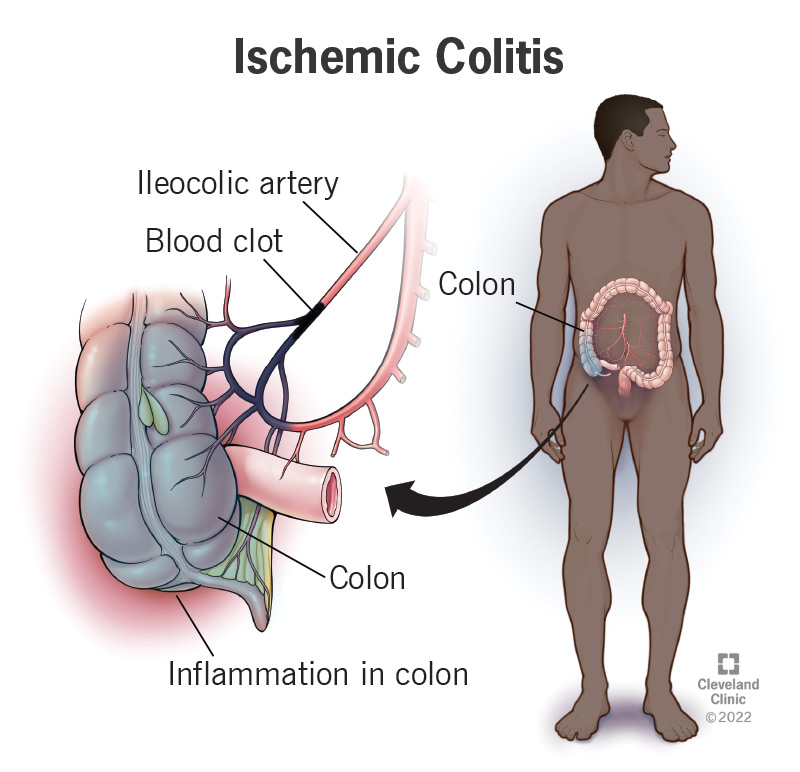
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/Images/org/health/articles/24513-ischemic-colitis)
Ischemic colitis is inflammation in your colon that’s caused by ischemia, which means reduced blood flow. Blood supplies oxygen to the tissues in your body. If something interrupts or diminishes the blood supply to certain tissues, they suffer damage from the lack of oxygen. Inflammation is your body’s response to this injury. It causes discomfort, swelling and bleeding, but it means your tissues are trying to repair themselves. Ischemic colitis mainly affects the inner lining of your colon (mucosa), usually in one section of it. But ischemia that’s more severe or lasts longer may do deeper damage to your colon.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Colitis means inflammation in your colon. Ischemic colitis is one of the less common ways that can happen. People often think of colitis in terms of chronic inflammatory bowel diseases, such as ulcerative colitis or Crohn’s disease. These are conditions that begin in the tissues of your colon itself. Ischemic colitis, on the other hand, is a problem that begins in your circulatory system. It may be related to low blood pressure or blood vessel diseases. Reduced blood flow in the arteries that supply blood to your colon causes inflammation in the tissues as a secondary effect. But your colon is otherwise well.
It most commonly affects people older than 60 and with a history of arterial disease.
Other potential risk factors include:
For most people, it’s a temporary problem affecting only a small part of your large bowel (colon). Inflammation causes temporary discomfort, but it clears up on its own when the cause of the ischemia resolves. Less commonly, it can be a more serious problem. Some people have repeat or chronic episodes of ischemic colitis in one area, which can cause scarring that narrows the colon (stricture). And if ischemia is severe enough, it can cause tissue death (gangrene). This raises the risk of life-threatening complications, such as perforation (a hole), infection and sepsis, and it requires emergency surgery to fix.
Advertisement
You might have:
Many things can interfere with the blood flow to your colon, usually temporarily. Often, the cause has already been resolved by the time it’s diagnosed. If you have a transient episode of ischemic colitis, your healthcare provider might not be able to definitively tell you what caused it. But they might have some good guesses, based on your health history and other conditions. Diseases affecting your circulatory system, including your heart and blood vessels, may cause reduced blood flow in the arteries that supply your colon. A blood clot might obstruct one of them, or something else might compress one from the outside.
The arteries that supply your colon — your superior and inferior mesenteric arteries — are extra sensitive to anything that causes your blood vessels to constrict (vasoconstriction). This includes physical triggers like colds, medical conditions that cause low blood pressure and certain drugs (vasoconstrictors). These arteries respond to low blood pressure by constricting vigorously. Scientists believe this may be a survival mechanism designed to direct reduced blood flow to your more vital organs, like your brain and heart. As a result, your colon may be deprived of blood flow while this stress response is activated.
Providers sometimes designate the causes of ischemic bowel disease as occlusive vs. nonocclusive. An occlusive cause is a blockage affecting one of your arteries. A nonocclusive cause is reduced blood flow without a blockage, such as from low blood pressure or narrowing of the arteries. A third cause is injury during surgery. While rare, this injury is a known risk of abdominal aortic aneurysm (AAA) repair. When this happens, it tends to be more severe than the other, more transient causes of ischemic colitis, and it can be life-threatening. It occurs in 2% to 3% of AAA surgeries, and the mortality rate among these is 50%.
The symptoms of ischemic bowel disease are common and nonspecific, so healthcare providers may have to rule out many other possible causes before making the diagnosis. They’ll take images of your colon and may test a sample of your blood for infections or other factors. Colitis in general may show up in your blood test as a high white blood cell count. When your healthcare provider suspects ischemic colitis, they might suggest a colonoscopy to confirm it. Ischemic colitis has distinctive features in colonoscopy imaging. Your provider can also take tissue samples through the colonoscope if necessary.
Advertisement
The treatment will depend on how severe it is and if you have any complications, such as infection in your abdominal cavity. Severe or complicated cases will require emergency surgery. Most cases can be managed medically. You’ll receive IV fluids and broad-spectrum antibiotics to treat or prevent infection. You may receive oxygen therapy to help increase your cardiac output and blood flow. Your healthcare provider will discontinue any medications that contribute to ischemic colitis. They’ll prescribe bowel rest, which means not using your digestive system for a while to let it heal. You’ll have a liquid diet or IV nutrition.
Other possible treatments may include:
Advertisement
If you’re recovering from an acute episode of ischemic colitis, your healthcare provider will recommend no food at first. After that, you may transition to a liquid diet and eventually a soft diet. Avoid foods high in fiber for now. The idea is to make your intestines work as little as possible while they’re healing. Digestion requires more blood flow and oxygen to the area, while bowel rest gives your body the chance to restore that blood supply. If you have long-term (chronic) ischemic colitis or another chronic condition that predisposes you to ischemic colitis, your healthcare provider may give you specific long-term guidelines.
Most people with acute ischemic colitis (75%) have a relatively mild and transient case that affects only the mucous lining in one segment. Most will recover fully with conservative treatment. A smaller percentage of people have a more complicated case that requires surgery. Those who have complications tend to be those with preexisting conditions, such as heart disease and kidney disease, which make surgery riskier and recovery more difficult. This group is statistically more at risk of unfavorable outcomes and death (about 40%), although the risk isn’t from ischemic colitis alone.
Advertisement
So many things can lead to ischemic colitis that it may not be possible to prevent all of them. However, it’s always a good idea to take care of your preexisting conditions, especially those that affect your heart, blood vessels and kidneys. Avoiding smoking or using recreational drugs and eating a heart-healthy diet may prevent these conditions from worsening or causing complications. Strenuous exercise can also lead to ischemic colitis (“runner’s colitis”) by stressing your heart’s capacity to pump enough blood. If you’re an endurance athlete, staying well-hydrated can help prevent this.
Ischemic colitis can be mystifying to those who experience it, and it can take time for healthcare providers to diagnose it too. When your symptoms are in your intestines, nobody suspects cardiovascular problems first. Once the diagnosis is made, you may need to spend some time in the hospital, but most of the time you can expect a full and speedy recovery. Ischemic colitis can sometimes be more severe, though, so don’t hesitate to seek care for your symptoms or to let your provider know if they aren’t improving.

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
If you have issues with your digestive system, you need a team of experts you can trust. Our gastroenterology specialists at Cleveland Clinic can help.
