An implantable cardioverter defibrillator (ICD) is a device that monitors your heart and treats abnormal heart rhythms when needed. It’s surgically placed under your skin and connects to your heart with thin wires (leads). The battery-powered device can deliver an electric shock to correct life-threatening arrhythmias and treat sudden cardiac arrest.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
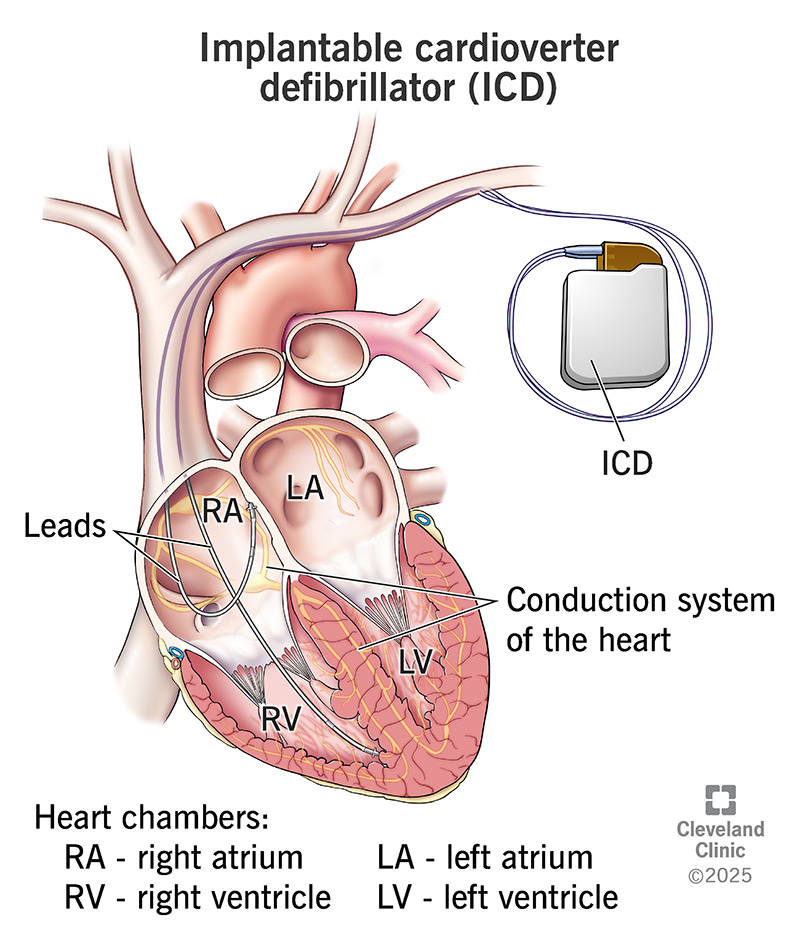
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/implantable-cardioverter-defibrillator)
An implantable cardioverter defibrillator (ICD) is a device that fixes life-threatening irregular heart rhythms (arrhythmias). It constantly monitors your heart. If it senses that your rhythm is one of the abnormal, life-threatening ones, it sends an electrical shock to your heart to correct it. Many ICDs have a built-in pacemaker, too.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
A surgeon places an ICD under the skin on your chest. It has a pulse generator and a thin wire called a lead. You may have more than one lead if the ICD is also meant to function as a pacemaker. The pulse generator is about the size of a stopwatch. It contains a battery and electrical circuits that read your heart’s electrical activity. The leads go into your heart chambers to monitor your rhythm and deliver a shock if need be.
A subcutaneous ICD is a different type of ICD. It has a thin wire that travels under your skin to the outside of your heart. Its purpose is to deliver a shock to correct dangerous heart rhythms if they occur.
ICDs can:
Other names for an ICD include:
You may need an ICD if you’re at high risk of sudden cardiac death from an abnormal heart rhythm. Conditions that can cause this include:
Advertisement
Before you get an implantable cardiac defibrillator, your healthcare provider may ask you to:
The type of procedure you have depends on your health and other treatments you need at the same time.
The transvenous approach is the most common for ICD implantation. It involves a small incision (cut) near your collarbone. Your healthcare provider threads the leads through veins to get to your heart. In some cases, implantation requires open-heart surgery.
ICD implantation processes can vary widely. But in general, your provider will:
The procedure typically takes a couple of hours.
An ICD can treat life-threatening arrhythmias and sudden cardiac arrest. It can also provide important information about your heart to your cardiologist.
ICD implantation is generally safe. But as with any surgery, the procedure comes with risks, including:
After ICD implantation, you may feel tired and sore, especially near the incision. Your healthcare provider may suggest pain medications to make you more comfortable.
Many people go home the day after surgery. Depending on your health and the type of procedure you had, you may have to stay in the hospital for a few days.
Before you go home, your healthcare provider may test the ICD system again.
Most people need only one shock to restore a normal heart rhythm. But you may get two or more shocks in 24 hours. Your provider can adjust the frequency and intensity of shocks depending on the situation.
You should let your provider know if you have any shocks. It could mean you’re having a cardiac emergency or that the ICD isn’t functioning properly.
Advertisement
If you have an ICD, carry a card in your purse or wallet to alert emergency personnel. This will help them care for you if you have a medical emergency and can’t communicate.
Similarly, you should tell all your healthcare providers about your ICD. This includes dentists and imaging technicians. They may use equipment that can interfere with an ICD’s function.
Strong magnetic fields and some technology can interfere with an ICD’s function. Ask your healthcare provider if you should avoid or minimize:
Tell your healthcare provider if you develop any signs of infection, like:
Get medical help immediately if you receive several shocks from your ICD in a short time.
Advertisement
An ICD can be programmed to give low-energy or high-energy shocks. A low-energy shock can feel like a flutter or thump in your chest. High-energy shocks can be painful for a moment, like a blow to the chest.
ICD batteries last up to seven years. But this can vary depending on how often you’re receiving shocks. Your healthcare provider should check your ICD every three to six months.
Heart problems that put you at risk for sudden cardiac arrest can be scary. The good news is that an implantable cardiac defibrillator (ICD) may help protect your heart and life. Your healthcare provider will talk you through the procedure and what having an ICD is like.
Advertisement

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
When your heart rhythm is out of sync, the experts at Cleveland Clinic can find out why. We offer personalized care for all types of arrhythmias.
