Ventricular fibrillation (or v-fib, for short) is an abnormal heart rhythm that makes your lower heart chambers move quickly and randomly. This life-threatening condition affects your lower heart chambers’ ability to pump blood. You need immediate medical care for this condition.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
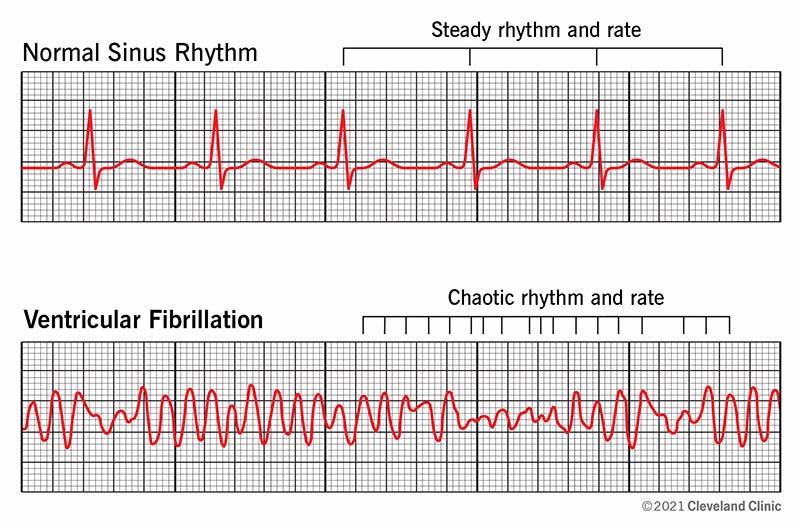
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/21878-ventricular-fibrillation-illustration)
Ventricular fibrillation (v-fib or VF, for short) is the most common deadly arrhythmia. With this irregular heart rhythm, your heart’s lower chambers (ventricles) beat in an erratic way. They quiver or twitch instead of expanding and squeezing. This means they can’t pump blood as they should.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
When blood stops flowing for this reason, you typically have just a few seconds before you pass out. This is called cardiac arrest, which is usually fatal in a few minutes without immediate care.
If you see someone collapse, you might feel scared and not know what to do. The best way to help them is to call 911 or your local emergency number.
Just before v-fib, you may have these ventricular fibrillation symptoms:
Someone who has this condition will collapse with little or no warning and won’t respond or react when you try to wake them. They’ll also gasp for breath or stop breathing.
Ventricular fibrillation causes include:
Advertisement
In addition to existing heart conditions like coronary artery disease, the following raise your risk of v-fib:
It’s rare for people to make a complete recovery from v-fib. Contact your provider for help managing lingering issues after ventricular fibrillation.
Complications of ventricular fibrillation rhythm include:
A provider can confirm a ventricular fibrillation rhythm with an electrocardiogram (EKG), especially after resuscitating you from cardiac arrest. They can also diagnose it during cardiac arrest if you have a cardiac monitor on or an implanted cardiac device.
They’ll also work to find out what caused ventricular fibrillation. A provider will collect your medical history and do a physical exam. They may order several other tests, like blood tests, an echocardiogram, a cardiac MRI (magnetic resonance imaging) or a coronary angiogram with a cardiac catheterization.
This condition is a life-threatening medical emergency. Every minute counts. Ventricular fibrillation treatment starts with calling your local emergency number. The following actions can help save the life of someone who’s in sudden cardiac arrest because of v-fib:
If you survive a ventricular fibrillation rhythm, you’re at a higher risk of it happening again. Your healthcare provider will run tests to find out what caused it and what follow-up options will work best to keep it from happening again. For example, if medications or an electrolyte imbalance caused your v-fib, a provider can stop the medicines or correct your electrolyte imbalance.
You also may need treatments like:
Advertisement
A provider may suggest procedures like ablation or cardiac sympathetic denervation. These less common treatments destroy signal pathways.
Like any medication, antiarrhythmics have side effects. Work with your provider to find the medicine that’s best for you.
When an ICD fires in response to v-fib, you may experience pain or shock.
Your outlook with ventricular fibrillation depends on how quickly someone helps you. With quick treatment, up to 50% of people can survive. Without immediate treatment, a ventricular fibrillation rhythm is fatal. For each minute you wait for defibrillation, your chance of survival drops by 7% to 10%.
Defibrillation only works on 30% of people who have heart failure. Heart failure is often fatal, even for those who have a successful defibrillation.
Most cases of v-fib start out as another type of ventricular arrhythmia. If you show symptoms of an abnormal heart rhythm in your lower heart chambers, a provider can monitor your rhythms. Finding these issues early can help prevent you from developing ventricular fibrillation.
If someone in your family has a type of arrhythmia that families can pass down to each other, ask about genetic testing. Testing people who may be at risk can help them take steps to prevent dangerous heart rhythms.
Advertisement
Since heart attacks are the top cause of ventricular fibrillation, preventing a heart attack can prevent v-fib, as well. You can do this by making lifestyle changes like:
No. Ventricular fibrillation is an abnormal beating rhythm in the lower chambers of your heart. A heart attack is different. It happens because of blockages in the blood vessels that supply your heart with enough oxygen to keep pumping. But a heart attack can cause ventricular fibrillation.
Ventricular tachycardia and ventricular fibrillation are closely related conditions. In ventricular tachycardia, your heart’s lower chambers are beating much faster than they should. But the overall process is happening in the right order. In ventricular fibrillation, your heart’s beating process isn’t happening in the right order.
Both conditions are life-threatening because they can lead to collapse and sudden cardiac arrest. In emergencies, defibrillation typically treats both issues. The long-term treatment for both is usually an implanted cardioverter defibrillator (ICD).
Advertisement
You may find it hard to talk about ventricular fibrillation and sudden cardiac arrest, especially if you continue to have health issues from them. Your healthcare provider can give you guidance that can help you better understand your situation. Don’t be afraid to ask questions or ask for help as you focus on living your best life.
Learn more about the Health Library and our editorial process.
Cleveland Clinic's health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability, and up-to-date clinical standards.
Cleveland Clinic's health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability, and up-to-date clinical standards.
When your heart rhythm is out of sync, the experts at Cleveland Clinic can find out why. We offer personalized care for all types of arrhythmias.
