A heart attack is when blood flow to your heart is suddenly reduced, leading to heart muscle damage. It’s usually due to blood clots that form on plaque in your heart’s arteries. Symptoms include chest pain/discomfort, shortness of breath, profuse sweating or nausea. Call emergency services if you have these symptoms. Quick care can save your life.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
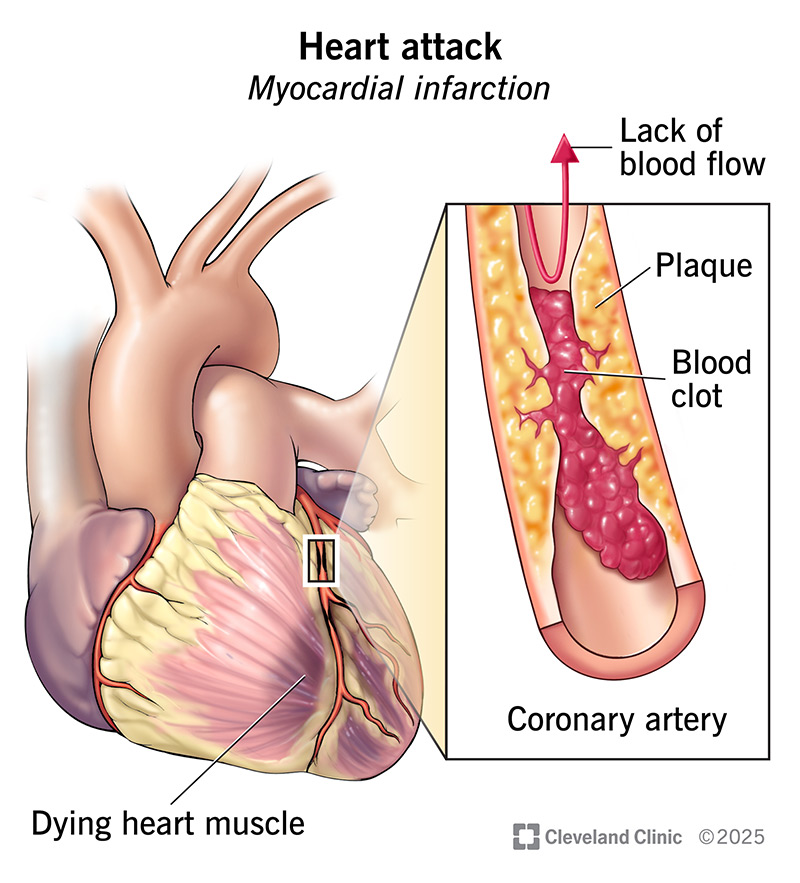
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/16818-heart-attack.jpg)
A heart attack is a medical emergency because your heart isn’t receiving enough oxygen-rich blood. This is often due to a blockage in one of your heart’s arteries (coronary arteries). Without steady blood flow, areas of your heart muscle can begin to die. This keeps your heart from pumping normally and reduces blood flow to the rest of your body.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
You may also hear a heart attack referred to as a myocardial infarction or MI.
Call 911 or your local emergency services number if you think you’re having a heart attack. While they send help, ask if you should take an aspirin. Don’t drive yourself to the hospital or let someone else drive you. First responders can start treating you as soon as they arrive. They can also send word to the nearest hospital that you’re on your way. This saves valuable time.
The two main types of heart attacks are:
You might also hear your provider use these terms:
Advertisement
A heart attack can feel like crushing chest pain, but not always. You might notice pressure, squeezing or heaviness in your chest. At times, it can be hard to diagnose because it may also feel like you’re having indigestion or heartburn. The chest discomfort usually lasts at least 10 minutes.
Symptoms may not hit you all at once. You may have early warning signs that start gradually. For example, you may notice mild chest discomfort with usual activities, such as climbing stairs or taking a brisk walk.
In general, the typical signs and symptoms of a myocardial infarction include:
It’s possible to have a heart attack without feeling chest pain. Some people only have shortness of breath, nausea or sweating. You might hear this called a “silent heart attack.” That’s because it doesn’t have the traditional symptoms. But it’s still a heart attack. And you still need care right away.
The most common cause of a heart attack is plaque buildup in your coronary arteries — a condition known as coronary artery disease. The plaque is most dangerous when its surface wears away or breaks open. Blood clots are drawn to that area. The clots can partly or completely block blood flow, leading to a heart attack.
It’s also possible for the plaque to take up so much space that there’s very little room for blood to get through. This severe narrowing reduces blood flow to your heart and may lead to a heart attack.
Other heart attack causes include:
Advertisement
Your risk of a heart attack goes up if you:
You can’t do much about certain things, like aging or family history. But there’s still a lot you can do to lower your risk. From eating heart-healthy foods to exercising regularly, it all adds up. A healthcare provider can also calculate your risk of heart problems and tailor advice to your needs.
A myocardial infarction can damage your heart, leading to complications like:
Advertisement
Besides its effects on your body, a heart attack also raises your risk for depression. This can make it hard for you to keep up with your daily routine, including rehab and other health check-ups.
A heart attack diagnosis needs to happen fast. It usually starts when first responders reach you and continues in the ambulance and emergency room. Healthcare providers use two key tests to see if you’re having a heart attack, and if so, what type:
Providers in the ER will talk to you about your symptoms, if you’re able to speak. They might also ask someone who was with you to describe what happened.
You may need more tests to check your heart function, rule out other causes of chest pain and check for complications. Possible tests include:
Advertisement
Treatment focuses on getting blood flowing to your heart again as soon as possible. Usually, this means you have a procedure to clear the blockage from your coronary artery. The sooner this happens after your symptoms start, the more it can help you. You’ll likely also need several medicines to help your heart work better and lower your risk of more problems.
There are three main ways healthcare providers can restore blood flow to your heart:
Medicines you may need as part of your heart attack treatment include:
Your heart attack symptoms should start to go away as you receive treatment. You’ll likely feel tired and weak during your hospital stay and for several days after.
Your healthcare provider will tell you how long you can expect to stay in the hospital, usually anywhere from a few days to a couple of weeks. It depends on the treatments you receive and how your body responds. In general, PCI has a shorter hospital stay than CABG.
Heart attack recovery takes anywhere from two weeks to three months. Your provider will advise you on how to take care of yourself during this time. They’ll also say when it’s safe to go back to work, drive and do other things.
Cardiac rehab is a key part of recovery. This 12-week program includes supervised exercise, nutrition advice and more. It helps you feel better faster and lowers your risk of future heart problems.
Follow-up visits are vital after a heart attack. After you finish cardiac rehab, you’ll see your provider every three months for the first year. Then, you’ll get down to every six months and eventually, once a year. At these visits, your provider will:
Call your provider if you have:
The treatment you receive for a heart attack doesn’t end when you leave the hospital. Once you have a heart attack, your risk for having another goes up. This means you’ll need to take prescribed medicines and make changes to your daily habits.
Today, many people survive a heart attack. But lots of things affect your outlook, including how much heart damage occurred, your age and underlying conditions. That’s why it’s so important to work closely with your provider. They’ll do everything possible to protect your heart and help you live a long life.
A heart attack is a life-changing event. One minute, you’re going about your routine. The next minute, you’re rushed to the hospital. You’ll probably never forget the emotions of that day. But that doesn’t mean you have to carry the fear or anxiety with you.
Recovering from a heart attack takes time. As your body starts healing, your thoughts and feelings might need some time to catch up, too. But if you still find yourself feeling down or anxious several weeks after your heart attack, talk to your provider. They can offer treatments to help.

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Whether you need stitches, a broken bone set or think your appendix might be causing your abdominal pain, Cleveland Clinic’s emergency medicine team is here to help.
