A STEMI is a severe type of heart attack in which there’s a complete blockage in one of your coronary arteries. This stops blood flow to part of your heart muscle. A STEMI is a medical emergency. The longer the blockage lasts, the greater the damage to your heart. Procedures and medicines can restore blood flow and improve your chances of survival.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
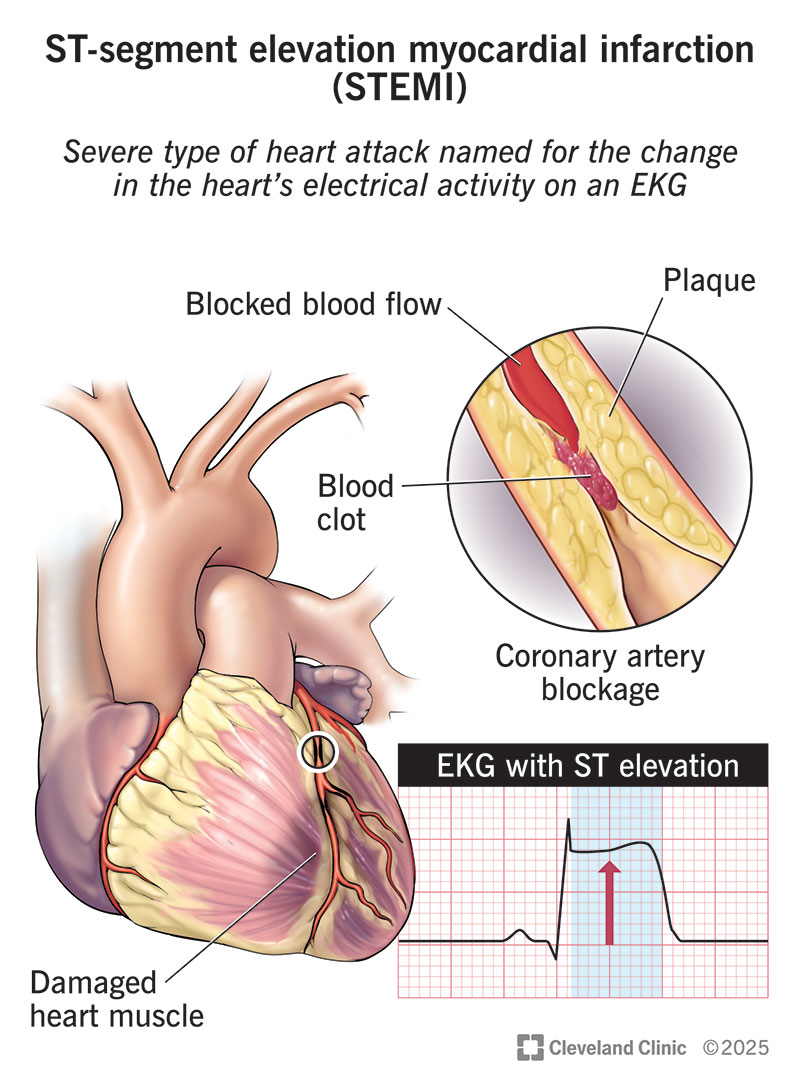
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/22068-stemi-heart-attack-illustration)
An ST-segment elevation myocardial infarction (STEMI) is a type of heart attack that happens when one of your coronary arteries is totally blocked. Such a blockage stops blood flow to your lower heart chambers (ventricles) and affects their electrical activity. This makes a distinct pattern on an electrocardiogram (ECG/EKG) graph, which is how this condition got its name.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
STEMIs have a greater risk of serious complications and death than heart attacks that result from a partial blockage (NSTEMI). But you can’t tell the difference based on how you feel. And a partial blockage can quickly turn into a total one. All heart attacks are medical emergencies.
Call 911 (or your local emergency service number) right away if you think you’re having a heart attack or have any early warning signs. Every minute matters. Delays in seeking care can lead to permanent heart damage or death.
STEMIs are common and affect hundreds of thousands of people in the U.S. each year. Even though more people survive than in the past, STEMIs are still a leading cause of death globally.
Healthcare providers name STEMIs based on which coronary artery is blocked. You might hear them say:
Advertisement
STEMI symptoms are the same as those for any type of heart attack and include:
Seek emergency care immediately if you have these symptoms. Call 911 or your local emergency services number. Never drive yourself or let someone else drive you.
This is because first responders can start caring for you in the ambulance. They can also share information with healthcare providers at the hospital before you arrive. This saves time and lets you get lifesaving care as quickly as possible.
A STEMI happens when a blood clot completely blocks blood flow in one of your heart’s arteries. The clot typically forms over plaque — a mix of fat and other stuff — that breaks open or wears down inside the artery. This type of complete blockage is the most severe form of coronary artery disease.
Your risk for a STEMI, or any type of heart attack, goes up if you:
A STEMI prevents oxygen-rich blood from nourishing your heart muscle. The longer the blockage lasts, the more damage it can cause. Areas of your heart muscle may start to die.
Possible complications include:
STEMI diagnosis begins as soon as first responders reach you. They’ll check your vital signs and do an EKG — a test that shows how your heart is beating. If the EKG shows a pattern called “ST-segment elevation,” it usually means one of your coronary arteries is totally blocked. That means your heart muscle is getting damaged and needs treatment fast.
Other tests that help providers diagnose a STEMI and its complications include:
Providers also review your medical history and may ask about your symptoms if you’re able to speak.
Advertisement
The goal of STEMI treatment is to get blood flowing to your heart again as soon as possible. This usually involves having a procedure called percutaneous coronary intervention (PCI) to open your coronary artery. You’ll also need medications to help your heart work better and lower your risk of complications.
Treatments to restore blood flow include:
Medicines you may need include:
Advertisement
You’ll start taking these in the hospital. Your provider will adjust your doses as needed. They’ll tell you exactly which medicines you need to keep taking at home, and why.
STEMI symptoms should decrease as you receive emergency care. How long you stay in the hospital depends on the treatments you need and your overall condition. Most people go home within a week or two. It’s common to feel weak or tired for several days after you return home. You should gradually regain your strength and return to your usual activities over the next two to three months.
Cardiac rehab is an important part of your recovery. During this 12-week program, providers help you with exercise, nutrition and more. This strengthens your heart and lowers your risk of more issues down the road.
Your healthcare provider will schedule regular follow-up visits with you. These start during your recovery and continue for the rest of your life. Once you’ve had a STEMI, you have a greater risk of having another heart attack. That’s why follow-ups are vital.
Call your provider any time you have new symptoms or just feel different than usual.
If chest discomfort or other STEMI symptoms return, call 911 or your local emergency services number.
Advertisement
Your outlook depends on many things. The most important factor is how much damage there is to your heart muscle from the STEMI. That’s why it’s so critical that you seek medical care quickly if you think you’re having a heart attack.
The good news: Treatments have come a long way. Many people live long lives after a STEMI — sometimes, even longer than people who haven’t had one. One study showed that those who survive 90 days after their STEMI have a good chance of living at least 10 years longer.
The risk of death within 10 years of a STEMI goes up if you:
You can improve your chances of survival by:
Most of us have heard of a heart attack. But a STEMI? That might be new. You may be learning about STEMIs because you’ve just had one. Or maybe a loved one did. So, you likely know how serious they are — and the emotions that can come along with the experience.
As the days go on, take the time to learn more about the condition. Talk to your provider about how you can lower your risk of repeat heart attacks. And don’t expect yourself to be at full strength overnight. A STEMI is serious. Your body and mind need time to recover. It’s OK to slow down and let others help you. This is also a good chance to educate others about heart disease and how they can lower their risk.

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
When your heart needs some help, the cardiology experts at Cleveland Clinic are here for you. We diagnose and treat the full spectrum of cardiovascular diseases.
