Brain tumors can be malignant (cancerous) or benign (noncancerous) and can affect children and adults. But whether they’re cancerous or not, brain tumors can impact your brain function if they grow large enough to press on surrounding tissues. There are several treatment options for brain tumors.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Video content: This video is available to watch online.
View video online (https://cdnapisec.kaltura.com/p/2207941/sp/220794100/playManifest/entryId/1_vk4q59ws/flavorId/1_5f3sgelj/format/url/protocol/https/a.mp4)
Learn about primary brain tumors, a tumor that grows on your brain.
A brain tumor is an abnormal growth or mass of cells in or around your brain. Together, spinal tumors and brain tumors are called central nervous system (CNS) tumors.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Brain tumors can be malignant (cancerous) or benign (noncancerous). Some tumors grow quickly, while others are slow growing.
Only about one-third of brain tumors are cancerous. But whether they’re cancerous or not, brain tumors can impact brain function and your health if they grow large enough to press on surrounding nerves, blood vessels and tissue.
Tumors that develop in your brain are called primary tumors. Tumors that spread to your brain after forming in a different part of your body are called secondary tumors, or metastatic brain tumors. This article focuses on primary brain tumors.
Researchers have identified more than 150 different brain tumors.
Healthcare providers categorize primary tumors as glial (composed of glial cells in your brain) or non-glial (developed on or in the structures of your brain, including nerves, blood vessels and glands) and benign (noncancerous) or malignant (cancerous).
Many types of brain tumors can also form in your spinal cord or column.
Types of brain tumors that are usually benign include:
Advertisement
Approximately 78% of cancerous primary brain tumors are gliomas. These tumors develop in glial cells, which surround and assist nerve cells. Types of gliomas include:
Medulloblastoma is another type of cancerous brain tumor. These tumors are fast growing and form at the base of your skull. They’re the most common cancerous brain tumor in children.
Brain tumors can affect anyone. They're slightly more common in males.
Meningioma, which is usually benign, is the only type of brain tumor that’s more common in females.
The most serious type of brain tumor, glioblastoma, is becoming more common among people who are as the general population ages.
Primary brain tumors (tumors that originate in your brain) are uncommon. Only about 5 per 100,000 people are diagnosed with a primary brain tumor each year in the United States.
About 4,100 children under the age of 15 are diagnosed with a brain or central nervous system tumor each year in the United States.
Brain tumors — whether cancerous or not — can cause serious problems. This is because your skull is rigid and doesn’t provide room for the tumor to expand. Also, if a tumor develops near parts of your brain that control vital functions, it may cause symptoms, such as:
Brain tumors can cause problems by:
However, some people have brain tumors that never cause symptoms or grow large enough to compress surrounding tissues.
Advertisement
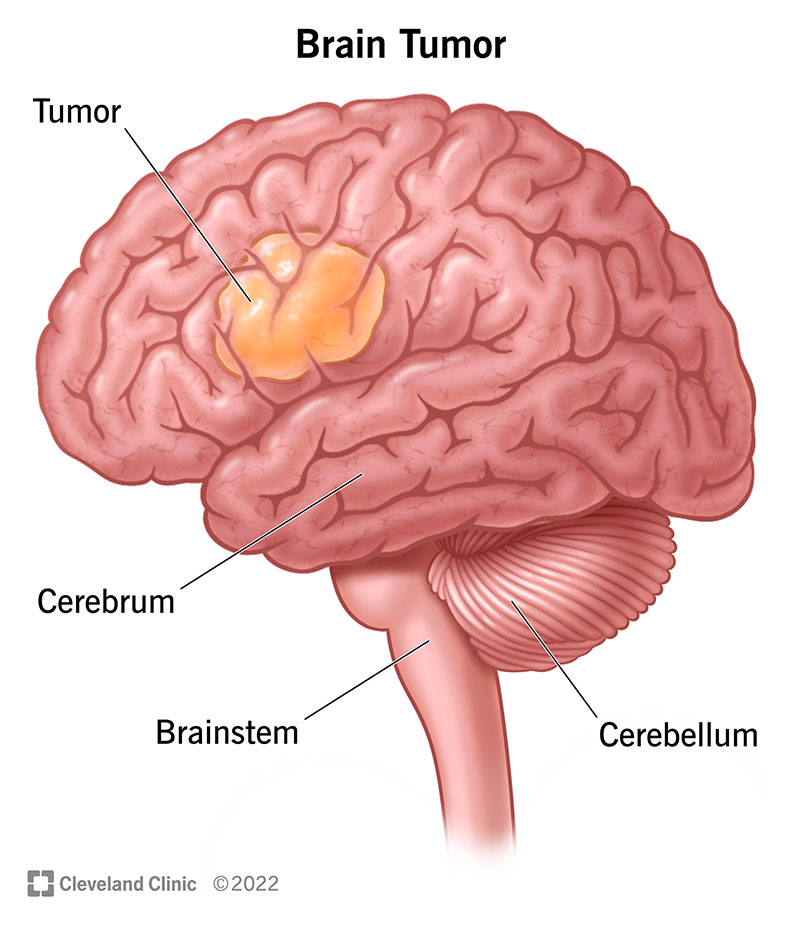
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/6149-brain-tumor)
Some people who have a brain tumor experience no symptoms, especially if it’s very small.
Signs and symptoms of a brain tumor vary depending on the tumor’s location, size and type. They can include:
It’s important to see your healthcare provider if you’re experiencing these symptoms.
Researchers know brain tumors develop when certain genes on the chromosomes of a cell are damaged and no longer function properly, but they aren’t sure why this happens. Your DNA in your chromosomes tells cells throughout your body what to do — it tells them when to grow, when to divide or multiply and/or when to die.
When brain cell DNA changes, it gives your brain cells new instructions. Your body develops abnormal brain cells that grow and multiply faster than normal and sometimes live longer than normal. When that happens, the ever-growing crowd of abnormal cells takes over space in your brain.
Advertisement
In some cases, a person may be born with changes in one or more of these genes. Environmental factors, such as exposure to large amounts of radiation from X-rays or previous cancer treatment, may then lead to further damage.
In other cases, the environmental injury to the genes may be the only cause.
There are a few rare, inherited (passed down from parent to child) genetic syndromes that are associated with brain tumors, including:
Only about 5% to 10% of people with brain tumors have a family history of a brain tumor.
Diagnosing a brain tumor can be a complicated process and may involve several specialists. In some cases, though, healthcare providers may discover a brain tumor when performing imaging tests for another medical issue.
If you’re experiencing symptoms of a brain tumor, your healthcare provider will perform a physical exam. They’ll also ask questions about your:
Advertisement
They may also perform a neurological exam, which involves looking for changes in your:
These changes can point to the part of your brain that may be affected by a tumor.
If your healthcare provider suspects you may have a brain tumor, a brain scan, most often an MRI, is usually the next step.
Healthcare providers use several tests to diagnose a brain tumor, including:
Brain tumor treatment depends on several factors, including:
Benign (noncancerous) brain tumors can usually be successfully removed with surgery and don’t usually grow back. It often depends on if your neurosurgeon can safely remove all of the tumor.
Treatments that are fairly well tolerated by the brains of adults, such as radiation therapy, may prevent the normal development of a child’s brain, especially in children younger than age five.
Healthcare providers often use a combination of therapies to treat a tumor. Your treatment options might include:
Other treatments that help with symptoms caused by brain tumors include:
The prognosis (outlook) for people with brain tumors varies greatly. Factors that affect the prognosis include:
In many cases, healthcare providers can successfully treat a brain tumor. Some people live active and fulfilling lives with brain tumors that don’t cause symptoms. For some people, brain tumors can recur (return) after treatment. If this happens to you, you may need to continue treatments, including chemotherapy or radiation, to keep the tumor from growing or spreading.
Survival rates are different for each type of brain tumor and vary based on your age, race and overall health. Survival rates are estimates based on averages. The five-year survival rate tells you what percent of people live at least five years after they’re diagnosed with a brain tumor. The five-year survival rates for meningioma, the most common type of benign (noncancerous) primary brain tumor, are:
Survival rates vary widely and depend on several factors. Talk with your healthcare provider about what to expect with your diagnosis.
Unfortunately, you can’t prevent a brain tumor. You can reduce your risk of developing a brain tumor by avoiding environmental hazards such as smoking and excessive radiation exposure.
If you have a first-degree biological relative (sibling or parent) who has been diagnosed with a brain tumor, it’s important to tell your healthcare provider. They may recommend genetic counseling to see if you have an inherited genetic syndrome that’s associated with brain tumors.
If you’ve been diagnosed with a brain tumor, you’ll need to see your healthcare team regularly to receive treatment and monitor your symptoms.
You should see your healthcare provider if your brain tumor symptoms get worse or you have new symptoms.
Even after brain tumor treatment, you should follow up with your healthcare provider regularly.
If you’ve been diagnosed with a brain tumor, it may be helpful to ask your healthcare provider the following questions:
Learning you have a tumor in your brain can be scary and stressful. Not all brain tumors are cancerous, though — in fact, about two-thirds of them are benign. However, they can still cause problems for your brain. Know that your healthcare team will develop an individualized and thorough treatment plan to help treat the tumor and improve your quality of life.

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
When you learn you have a skull base tumor, you’ll want the best care from the best providers. Cleveland Clinic is here to help.
