A cardiac catheterization is a low-risk, diagnostic procedure. A healthcare provider uses it to see how well your heart is working and what kind of treatment you may need. Using a long, narrow tube (catheter), a provider goes through a blood vessel in your leg or arm to get to your coronary arteries.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Cardiac catheterization (cardiac cath or heart cath) is an invasive imaging procedure that allows your healthcare provider to evaluate your heart function. Your provider puts a catheter (tiny tube) into a blood vessel in your arm or groin. From there, the tube goes to your heart and can show your coronary arteries and/or pulmonary artery so your provider can look at structural issues.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
The purpose of cardiac catheterization is to find problems with how your heart is working and its blood flow. Sometimes, during a heart cath, a provider may use other procedures to fix issues. For example, they could fix a heart issue you were born with or replace your heart valve without doing open-heart surgery.
Cardiac catheterization isn’t surgery. Providers don’t make a large cut (incision) for cardiac cath. Also, the recovery time is much shorter than for surgery. In some cases, your provider may recommend surgery afterward, depending on the results of your procedure.
A specially trained cardiologist and a team of cardiology fellows, nurses and technicians will perform your cardiac catheterization.
The two types of cardiac catheterization are:
Cardiac catheterization is used to:
Advertisement
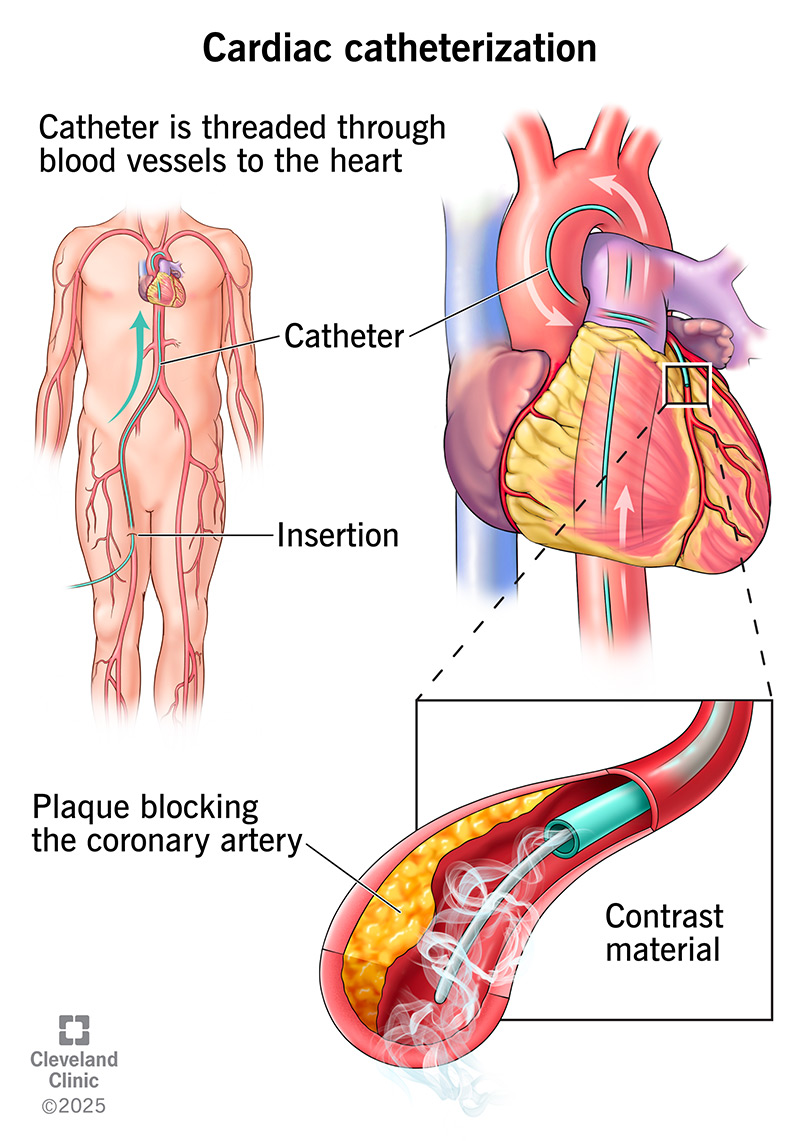
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/16832-cardiac-catheterization)
A provider uses contrast material to outline your vessels and heart chambers in images. They create X-ray movies (coronary angiogram) as the contrast material moves through your heart.
Digital photos of the contrast material allow your provider to:
In some cases, your healthcare provider may want to get better detail by using other imaging procedures during your cardiac cath. These may include:
Your provider may also want to perform procedures during your cardiac cath. These nonsurgical treatments may include:
A heart catheterization procedure that’s just looking at your coronary arteries generally takes 30 minutes. This can take more or less time depending on the goal of the procedure.
But the preparation and recovery time add several hours to your appointment time. It may be five to nine hours or longer. You should plan on staying at the hospital all day for your procedure, even though you’re awake for it. If your providers decide to do an intervention, like an angioplasty, that can take longer — sometimes a couple of hours.
Before a cardiac catheterization, you can expect to:
Once you arrive, you’ll:
Advertisement
During your cardiac catheterization procedure, a healthcare provider will:
Your healthcare provider will remove the catheters and sheath after your procedure.
If you had a catheter in your arm for your cardiac cath, you can expect to:
Advertisement
If you had a catheter at your groin for your heart cath, your provider will:
For heart catheterization recovery, you’ll:
You can usually drive 24 hours after leaving the hospital. Depending on where the catheter was, you’ll need to avoid strenuous activities (including sports and lifting) for two to five days. Your healthcare provider can tell you when you can return to work.
Advertisement
During your recovery at home, you shouldn’t submerge the puncture site in water for a week. That means no swimming or taking baths. But you may shower 24 hours after the procedure.
Some of the possible cardiac catheterization risks include:
When you talk with your provider, ask questions to make sure you understand all of the potential risks and why they recommend the procedure.
Although cardiac catheterization isn’t surgery, you may consider it a serious procedure. But people rarely have complications from a heart cath. Providers perform more than one million cardiac catheterizations in the U.S. each year.
After completing your cardiac catheterization, your healthcare provider will have a lot of information they can use to decide your next step in treatment. Depending on the reason for your heart catheterization, your results can vary.
Your provider may:
Your healthcare provider may discuss your results with you right away. For something that takes more time, like a lab analysis of a tissue sample, it might take a few days to get results.
If your healthcare provider found a problem during the heart cath, they may schedule another procedure. With the information they gathered, they may start planning for a surgery.
Contact your healthcare provider after your cardiac catheterization if you have:
If you feel you’re having a heart attack or stroke, get help right away.
It can be scary to think about someone looking at your heart from the inside. But a cardiac catheterization isn’t surgery and your team will keep you comfortable. A heart cath provides valuable information your healthcare provider can use to decide their next steps. Collecting that information gets you one step closer to a treatment that’s best for you. Don’t hesitate to ask your provider any questions you have.
Learn more about the Health Library and our editorial process.
Cleveland Clinic's health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability, and up-to-date clinical standards.
Cleveland Clinic's health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability, and up-to-date clinical standards.
When your heart needs some help, the cardiology experts at Cleveland Clinic are here for you. We diagnose and treat the full spectrum of cardiovascular diseases.
