Moyamoya disease is a rare condition that affects the blood vessels in your brain. It can lead to brain bleeds and stroke in affected areas of your brain. There’s no cure for moyamoya disease. Treatment typically involves managing symptoms and preventing blood clots with medications. You may also need surgical bypass to supply more arteries to your brain for adequate blood flow.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
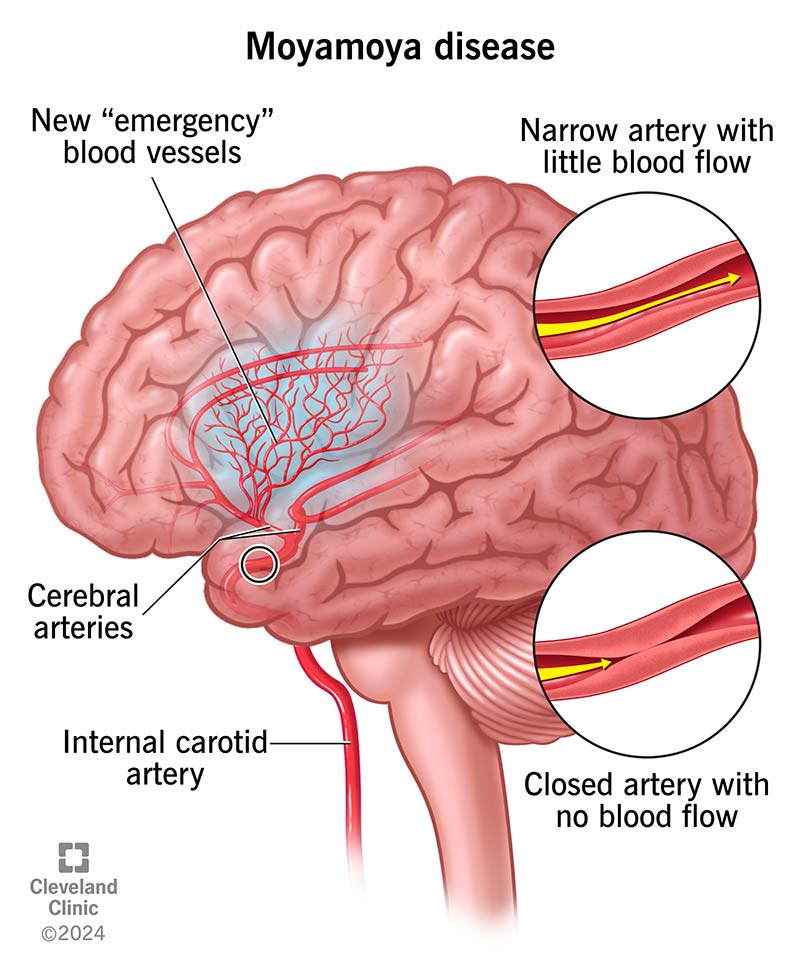
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/17244-moyamoya-disease)
Moyamoya disease is a type of cerebrovascular disease — a condition that affects the blood vessels in your brain. In moyamoya disease, at least one of your carotid arteries — and sometimes both — narrow or close. It also affects your front and/or middle cerebral arteries. These key arteries deliver blood and oxygen to the front two-thirds of your brain. When these blood vessels narrow, it blocks blood flow to your brain.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Over time, your brain forms new blood vessels to make up for the blood and oxygen lost from the blockage. But as these blood vessels are formed as emergency backup vessels, they’re smaller and often weaker than the blocked arteries. These smaller, backup arteries often can’t supply enough blood to your brain. This may lead to brain bleeds and stroke in the affected areas of your brain.
“Moyamoya” is a Japanese word that means “puff of smoke.” Japanese doctors discovered that the smaller backup vessels looked like curled-up puffs of smoke when they did blood vessel scans called angiograms. That’s why they used the term “moyamoya disease” to describe the condition.
Moyamoya disease is most common in Japan, where it affects about 5 in every 100,000 people. In the United States, the condition affects fewer than 5,000 people.
A lack of blood supply to your brain can lead to the symptoms of the disease. The first sign of moyamoya disease is often stroke or repeated transient ischemic attacks (TIAs). Healthcare providers may call these “mini-strokes.” Other moyamoya disease symptoms may include:
Advertisement
Researchers don’t know the exact causes of moyamoya disease. But there appear to be genetic and acquired forms of the condition. Researchers are still exploring genes that could get passed down from biological parents. There may be other factors, like inflammation or infection, that could cause the condition, too.
Sometimes, moyamoya disease occurs with other conditions and is called moyamoya syndrome or phenomenon. Examples of these other conditions include:
Researchers have discovered mutations, or changes, in one gene — RNF213 — that may be responsible for at least some cases of moyamoya disease. The RNF213 gene is responsible for producing a protein that may be involved in the development of blood vessels.
As many as 15% of people of Japanese descent with moyamoya disease have one or more biological family members with the condition. That’s a sign that the condition is likely genetic, but the inheritance pattern is unknown.
Moyamoya disease is rare. Although the genetic forms occur mostly in people of Japanese ancestry, healthcare providers see it more and more in people from other ethnic backgrounds.
For reasons that scientists don’t understand, moyamoya disease is two times more common in females.
You can get moyamoya disease at any age, but you’re more likely to get it if you’re between five and 10 years old or between 30 and 50 years old.
Complications of moyamoya disease may include:
A healthcare provider will perform a physical examination and ask you about your symptoms. If they suspect moyamoya disease, you may need the following tests:
Moyamoya disease is progressive. That means it will gradually get worse without treatment. Healthcare providers use the “Suzuki” stages to describe the severity of the disease. They’ll use the MRA test to help determine what stage of the disease you’re in. Suzuki stages include:
Advertisement
Moyamoya disease treatment involves managing your symptoms with certain medications. Your healthcare provider may recommend or prescribe medications like:
Advertisement
Medications can’t stop blood vessels from narrowing, so moyamoya disease may continue to worsen. Your healthcare provider may then consider moyamoya disease surgery. This is a type of bypass surgery that:
Your healthcare provider can discuss which method of moyamoya disease surgery would work best in your situation. They can also go over the side effects and possible complications of surgery.
For most people with moyamoya disease, the condition gets worse over time. They may also experience stroke as blood vessels narrow more and more. Without treatment, moyamoya disease can lead to stroke with severe neurological deficits. But some people remain stable for years without symptoms. Once symptoms start to develop, your provider may suggest bypass surgery.
Advertisement
With early diagnosis and prompt treatment, people with moyamoya disease can have a normal life expectancy. Without treatment, moyamoya disease can be fatal.
There’s no proven way to prevent genetic forms of moyamoya disease. But you can lower your risk of developing moyamoya syndrome by managing vascular risk factors and reducing your risk of atherosclerosis.
You may be able to relieve symptoms and avoid complications from moyamoya disease if you make sure to take your medications exactly as directed.
Get immediate medical attention if you experience any signs of a stroke.
The American Stroke Association uses the acronym F.A.S.T. to help people remember how to react:
Other symptoms of stroke include sudden:
Moyamoya disease is a rare condition that can lead to stroke and brain bleeds. Researchers don’t know the exact cause of the condition, but it appears to affect people of Japanese descent most often. If you have any of the symptoms of moyamoya disease, make an appointment with a healthcare provider. Prompt diagnosis and treatment are vital with moyamoya disease. It’s also important to recognize the signs of stroke, which need immediate medical attention.

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Sometimes strokes are a sign of other serious issues, like moyamoya disease. Cleveland Clinic offers personalized diagnosis and treatment to reduce your stroke risk.
