Gastric bypass surgery is a procedure that helps you lose weight. It’s weight loss treatment for people who have a body mass index (BMI) of 30 or more. It works by reducing the size of your stomach. You don’t need to eat as much food to feel satisfied. You’ll also need to make a commitment to eating well and being active.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
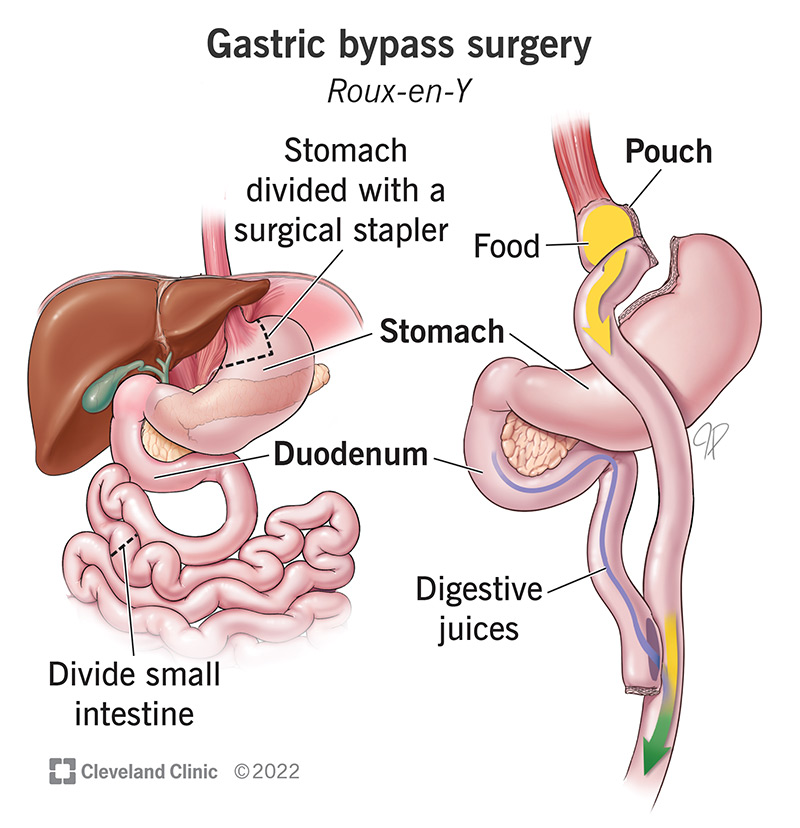
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/17157-gastric-bypasss-surgery.jpg)
Gastric bypass surgery is a type of bariatric surgery. It changes the size and shape of your stomach and small intestine. Gastric bypass surgery is a common treatment for obesity. The surgery divides your stomach into two sections. One is smaller than the other. This small section is called a stomach pouch. The stomach pouch is then connected to your small intestine. The new connection takes the form of a Y. This is why healthcare providers may use the French term Roux-en-Y gastric bypass surgery. Roux-en-Y means “in the shape of a Y.”
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Obesity is a disease that increases your risk for serious health issues. Gastric bypass surgery can help you lose weight and improve your health. This surgery can change your life, but it’s only part of that transformation. You need to be ready and able to commit to lifelong lifestyle changes. That’s how you lose weight and keep it off to improve your health.
The surgery changes how much food your stomach holds. Right after surgery, the small stomach pouch (your “new” stomach) will hold about 1 ounce of food. The average adult stomach can hold about 32 ounces of food. Eventually, the small pouch will be able to hold 8 ounces of food.
Gastric bypass surgery also affects how food moves through your small intestine. Food typically travels through 22 feet of small intestine to reach your large intestine. The surgery creates a shortcut so that food skips the first part of your small intestine and goes straight to the middle part. That shortens the digestion period. Your poop will look and smell different because it contains partially undigested food.
The surgery also makes lasting changes to your metabolism. Your metabolism is how your body turns food into energy. Gastric bypass surgery changes your metabolism by boosting certain hormones. Hormones are chemical messengers that control different functions in your body. Gastric bypass surgery appears to boost activity in some hormones. These hormones include:
Advertisement
Everyone’s situation is a bit different. Research shows people lose about 30% of their baseline weight after surgery. Baseline weight is how much you weigh before surgery. So, if you weigh 300 pounds before surgery, you’d lose about 90 pounds.
The first step is talking to a healthcare provider if you have concerns about your weight and your health. Your healthcare provider may refer you to a bariatric specialist to talk about surgery if your situation meets certain guidelines. The guidelines are based on body mass index (BMI). BMI estimates the amount of body fat you have based on your height and weight. There are different BMI classes. Providers consider surgeries like the gastric bypass for people who are:
There are other factors to consider. Gastric bypass surgery is major surgery. Your providers in the bariatric program you join will do tests to confirm you’re physically strong and healthy enough for surgery. They’ll discuss the lifestyle changes that you’ll follow after surgery. For example, you may need to avoid certain foods and be more active.
You and your providers will talk about these factors. If gastric bypass surgery is a good fit for you, your provider will explain the steps leading up to your surgery.
Your final preparations may begin about two weeks before your surgery. You’ll start a liquid diet of protein shakes and clear liquids. You’ll continue the liquid diet up until midnight on the day of your surgery. You can have clear liquids up to two hours before you arrive at the hospital.
You receive general anesthesia for this surgery so you’re asleep the entire time. You’ll have a breathing tube during the surgery. Your surgery team will remove it before you wake up. Steps in gastric bypass surgery are:
Advertisement
The procedure itself takes about two to three hours. Afterward, you’ll probably remain in the hospital for two days. You won’t be able to eat solid foods yet.
Gastric bypass surgery works when other weight loss programs aren’t successful. It makes it easier for you to manage your blood sugar, blood pressure and hunger pangs. The surgery may ease or reduce your risk of conditions like:
There are potential short-term and long-term risks with gastric bypass surgery. Short-term risks may include:
Potential longer-term complications are:
Recovery takes time. For example, you may need to avoid strenuous activities for two to four weeks after your surgery. Ask your care team to explain which activities you should avoid and what you can do as you recover.
Advertisement
Gastric bypass surgery changes what you eat and how much you eat:
Your healthcare team will help you get ready when it’s time to start eating solid food. They’ll share detailed information about what you should eat. In general, you should try to:
Your body will go through a lot of changes in the weeks and months after your surgery. Here are some suggestions that may help you to manage them:
Advertisement
Contact your surgeon if you have symptoms that could mean you have a surgical wound infection or bowel obstruction. The following symptoms are reasons to call your surgeon:
Success rates vary. But a 2021 study shows 92% of people had significant and long-term weight loss after surgery.
You’ll have a new normal after surgery. For example, you’ll feel full more quickly. That may change how and when you eat. You may have new limits on what you can eat. You might have to avoid sugary foods, too. But your new normal may also include being more active. It may mean you feel more comfortable in your body.
This surgery isn’t an option for everyone. You may not be able to have this surgery if:
Gastric bypass surgery isn’t a weight loss shortcut. It’s the beginning of a lifelong journey to better health. Talk to a healthcare provider if you’re living with obesity. They’ll ask about your efforts to lose weight. They’ll explain how gastric bypass surgery changes your body. They’ll also explain the lifelong lifestyle changes that you’ll need to make.
Gastric bypass surgery can be a big turning point in your weight loss journey. Your care team will be with you every step of the way.
Learn more about the Health Library and our editorial process.
Cleveland Clinic's health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability, and up-to-date clinical standards.
Cleveland Clinic's health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability, and up-to-date clinical standards.
If you have obesity and losing weight is an uphill battle, Cleveland Clinic experts can help you decide if bariatric surgery is an option.
