Neuromyelitis optica (NMO) is an autoimmune disease, meaning it happens when your immune system attacks parts of your nervous system. It most commonly affects your eyes, spinal cord and certain parts of your brainstem. Attacks of this condition are treatable, and it’s possible to manage and reduce the risk of future attacks.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
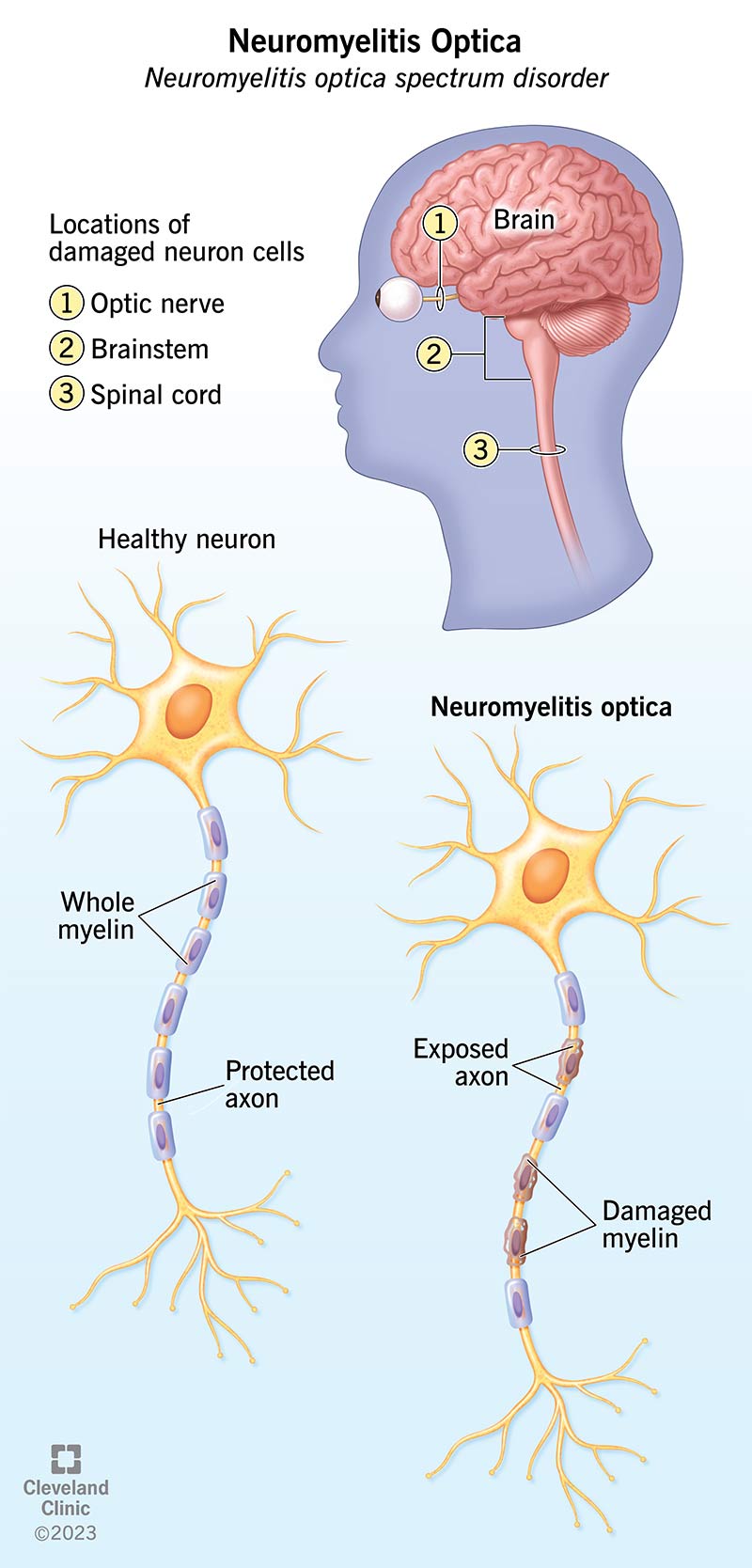
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/9858-neuromyelitis-optica)
Neuromyelitis optica (NMO) is a rare chronic condition that affects your eyesight and your ability to move. It’s an autoimmune disorder, meaning it happens because your immune system mistakenly attacks parts of your central nervous system.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
This condition has undergone name changes over the years. The condition’s original name, Devic’s disease, comes from Eugène Devic, the French neurologist who first described it. However, an international group of experts gave the condition its current name in 2015. This condition’s full, formal name is neuromyelitis optica spectrum disorder (NMOSD). But it’s still common for healthcare providers and other experts to simply call it neuromyelitis optica.
Experts previously thought that NMO was a rare type of multiple sclerosis (MS). However, they know now that it’s a separate condition.
NMO is much more likely to affect females, who make up about 80% to 90% of cases. It usually affects people between the ages of 30 and 40. NMO in children is very uncommon, making up only 5% or so of cases.
People of all races and ethnic backgrounds can develop NMO, but it doesn’t affect people of all backgrounds at the same rates. NMO affects people of African descent, especially African Caribbean descent, at higher rates. The Caribbean island of Martinique, a French territory, has the highest number of cases for the size of its population, about 10 per 1000,000 people. It can also disproportionately affect people of Asian descent.
Advertisement
NMO overall is rare. The average number of people with NMO per 100,000 is between 0.3 and 4.4. That means there are between 1,000 and 14,600 cases in the United States and between 24,000 and 350,600 cases worldwide.
To understand how NMO affects you, it helps to know a little about the makeup of your nervous system. Your nervous system consists of your brain and spinal cord (the optic nerves, which are the cranial nerves that allow you to see, are technically part of your brain also).
Together, your brain and spinal cord are known as the central nervous system. The network of nerves that branch outward throughout your entire body makes up your peripheral nervous system.
Your nervous system transmits information to and from your brain using chemical and electrical signals. Those signals travel through specialized cells known as neurons, which form incredibly complex connections to other neurons around them.
A key part of every neuron is an arm-like extension called the axon, which carries electrical signals to the synapses (pronounced sin-apps-is) at the end of the axon. These finger-like extensions are where the electrical signals in the neuron become chemical signals. The synapses connect and communicate with other nearby neurons.
Around the axon, there’s a thin, protective coating called myelin, which is made up of fatty chemical compounds. Myelin helps with conduction of electrical signals along the axon and protects it from damage. NMO is a demyelinating disease, meaning it involves the myelin coating of the axon. Without the protective myelin coating, the axon is vulnerable to damage and deterioration.
Damage from NMO tends to involve neurons in two specific areas: The optic nerve that connects your eyes to your brain, and your spinal cord, which is the central connection point for nerve signals to reach before heading to your brain. NMO can affect your spinal cord at different levels, and every nerve that connects to your spinal cord below the affected area of your spinal cord can show the effects.
NMO causes symptom “attacks,” meaning that the symptoms come and go. Attacks can last for days to months at a time. These attacks are often severe and can sometimes cause permanent damage. When this happens, the effects might be permanent even after an attack ends.
The symptoms of NMO break down into three categories (with more about these categories below):
Advertisement
Your eyes pick up light from the world around you and send signals through the optic nerve, the connection between your eyes and brain. Your brain then processes those signals, giving you your sense of sight.
Optic neuritis causes inflammation of the optic nerve, causing it to swell. There isn’t much space in that area of your head, so that swelling may put too much pressure on your optic nerve. Lying on an arm or leg can interrupt signals from your sense of touch, causing pain, tingling and numbness in the affected body part. Pressure on your optic nerve has a similar effect on your eyes.
The symptoms of optic neuritis can affect one or both eyes, and the timing of the symptoms can affect one eye after the other or both at the same time. The symptoms include:
Advertisement
Myelitis is inflammation of your spinal cord. That inflammation can cause swelling, which puts pressure on your spinal cord or the nearby spinal nerves. That can partially or totally block nerve signals that try to pass through the affected area. When myelitis disrupts all types of nerve signals, it’s known as transverse myelitis.
The symptoms of myelitis depend on where the swelling is and what parts of your spinal cord or spinal nerves it affects. If the swelling puts pressure on spinal nerves, the symptoms will affect areas that rely on those nerves to connect to your brain. If it puts pressure on your spinal cord, the symptoms will affect all parts of your body with spinal nerve connections below the area of pressure.
The symptoms of myelitis include:
Advertisement
While it’s common for multiple sclerosis (MS) to cause changes in your brain, it’s less common for this to happen with NMO. When it happens, it can disrupt how your brain handles certain processes in your body. If these disruptions happen in your hypothalamus or brainstem, they can cause severe or even dangerous problems.
The brainstem is the lowest section of your brain, found at the lower back of your skull. This section is critical for two reasons: It links your brain and spinal cord, and it controls autonomic processes. Your body’s autonomic processes are the functions that happen without you thinking about them (automatic). Examples include breathing, blood pressure, sweating and more.
If NMO affects your brainstem, it can cause the following symptoms:
Just above the brainstem is your hypothalamus. This structure also handles automatic body processes. When NMO affects it, this can cause other body systems to malfunction. A key example of this is NMO with narcolepsy symptoms (such as excessive daytime sleepiness).
So far, experts can only partly explain how or why NMO happens. The reasons they know about or suspect include:
NMO is an autoimmune condition, which means it happens when your immune system mistakenly attacks part of your own body. In this case, it attacks your optic nerves and/or your spinal cord.
There are two known autoimmune forms of NMO:
These immune system malfunctions happen for mostly unknown reasons. However, there's data that suggests these malfunctions can happen after having an infection. About 15% to 35% of people who develop NMO had some kind of infection just before they developed NMO symptoms. However, more study is necessary to confirm this.
Currently, experts don’t know why NMO happens in people who don’t have AQP4 or MOG antibodies, who make up about 13.5% of those with this condition. They classify these cases as “idiopathic,” meaning they happen for unknown reasons.
Additionally, some experts believe NMO that involves MOG antibodies is actually a separate disorder. However, more research is necessary on this and that formal recognition, as a separate disorder has yet to happen.
While NMO can happen on its own, it’s more likely to happen in people with other autoimmune or inflammatory conditions. However, more research is necessary before researchers can say whether or not these conditions can cause or contribute to NMO.
These conditions include:
Experts suspect that genetic factors can play a role in NMO. One reason they suspect this is because this condition is more common in people of certain ethnicities or racial backgrounds. Another reason is that about 3% of NMO cases involve people in the same families. While they don’t have evidence that NMO is a condition you can inherit, there might be genetic factors that make it easier to develop NMO.
Currently, there’s no evidence that NMOSD (NMO) can spread from person to person.
One of the most important differences between multiple sclerosis (MS) and NMO is that some test methods can confirm if a person has it. A healthcare provider can diagnose NMO using a combination of the following:
Other tests are also possible, as your healthcare provider may feel it’s important to rule out other conditions. Your provider can tell you more about the tests they recommend and why they recommend those tests.
NMO isn’t curable, but thanks to continuing research, this condition is treatable. Because NMO is an autoimmune condition, the main treatments take two forms: acute treatment and long-term management.
There are several drugs and treatments that can help treat NMO, including:
The side effects of the possible treatments can depend on many factors, including the specific drug, the severity of your condition and your medical history. However, one side effect of immune-suppressing drugs stands out: They lower your immune response.
Your immune system protects you from outside invaders like viruses, bacteria, fungi and parasites. It also controls and puts a stop to cells behaving badly. If cells in your body malfunction, your immune system’s job is to step in and destroy them (cancer is when cells malfunction and disguise themselves from your immune system, allowing them to reproduce uncontrollably without drawing your immune system’s attention).
Taking immune-suppressing drugs can help prevent NMO attacks, but it also reduces your body’s ability to fight certain infections, and it can raise your risk of certain types of tumors (both cancerous and noncancerous). If you take immune-suppressing drugs, you’ll need to take certain precautions to lower your risk of getting sick. You also may need certain vaccinations to prevent or limit the severity of infectious diseases, like COVID-19, influenza (flu) or pneumonia, which can be severe and potentially deadly if you have a suppressed immune system.
The treatment and recovery timeline can vary with NMO because many factors play a role. Your healthcare provider is the best source of information on this. They can tell you the timeline that’s most likely in your case, and what you can do to help that process.
If you have NMO, you can expect this condition to start without much warning. Some people have a respiratory infection or other kinds of illnesses just before developing it, but this only happens in about one-third (or less) of cases.
NMO attacks will cause vision problems, as they affect your optic nerves. That causes eye pain and disruptions in your vision. These usually get worse over a few days or weeks before peaking. These symptoms can be permanent if there’s significant damage to your optic nerves, but treatment can help avoid permanent damage.
NMO also affects the bottom-most area of your brain — the brainstem — and your spinal cord. That can cause automatic body processes to malfunction, leading to nausea and vomiting, uncontrollable hiccups and more.
When myelitis is severe, the pressure on your spinal cord can disrupt nerve signals to every part of your body at or below the affected area. That can cause muscle weakness, paralysis, loss of the sense of touch below a certain point and more. This can be severe if paralysis or muscle weakness affects muscles that control breathing. Quick treatment may keep these effects from becoming permanent.
NMO is an autoimmune condition, meaning it happens because your immune system mistakenly attacks parts of your own body. In this case, your immune system targets your nervous system. Treatment for this condition typically involves long-term suppression of your immune system. Unfortunately, that has the side effect of putting you at risk for infections. People who take immune-suppressing drugs need to take precautions to lower their risk of getting sick.
NMO causes attacks, which are flare-ups of symptoms. For people with AQP4 or MOG antibodies, NMO is a lifelong condition. Currently, people with this disorder often need to take immune-suppressing drugs for years or the rest of their lives to avoid attacks.
About 10% to 20% of people with NMO will have only one attack and never have another. This is most likely in people who don’t have AQP4 or MOG antibodies. However, there’s no way to predict this with total certainty, so your healthcare provider may still recommend taking these drugs to reduce the risk of having an attack.
In years past, NMO was a condition that had a very negative outlook. However, experts now know NMO is treatable, thanks to discoveries into the immune origins of this condition. Medications to manage this condition reduce the relapse rate by between 72% and 88%. The five-year survival rate for this condition is between 91% and 98%.
For people with NMO who experience multiple attacks, this condition is more likely to cause the loss of certain abilities, such as vision and movement. About 22% of people will fully recover from the effects of NMO, getting back all of their abilities. About 7% won’t recover at all. The remaining 71% will recover at least partly but may experience lingering effects.
NMO happens unpredictably and for reasons that healthcare providers still don’t fully understand. Because of this, there’s no way to prevent it or reduce your risk of developing it.
NMO is manageable, and your healthcare provider will help guide you on how to take care of yourself. Some of the most important things you can do include:
People taking immune-suppressing drugs have a higher risk of getting sicker from common infections, even ones that aren’t serious under ordinary circumstances. For someone taking immunosuppressants, you should call your healthcare provider if you have any of the following symptoms:
NMO and multiple sclerosis (MS) are conditions that have many similarities and overlapping symptoms. For years, experts mistakenly thought that NMO was a type of MS. But researchers now know that these are separate conditions.
A key difference between NMO and MS is that lab testing can help detect antibodies that cause NMO (though it can’t detect antibodies in all cases). The treatments for NMO and MS are also different, and some treatments for MS can make NMO symptoms worse.
Neuromyelitis optica (NMO) is a rare chronic disease that happens when your immune system attacks specific parts of your central nervous system. Experts previously thought this was a rare type of multiple sclerosis (MS) but now recognize it’s a separate condition. Unlike MS, lab testing can confirm most cases of NMO, allowing providers to recognize and treat it early.
Thanks to advances in research and medical understanding, NMO is a treatable condition. Attacks of this condition are treatable with medications or certain types of infusion procedures. Medications can treat and manage this condition in those who test positive for certain antibodies. That means people with NMO can manage their condition better and reduce the risk of future attacks.
Learn more about the Health Library and our editorial process.
Cleveland Clinic's health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability, and up-to-date clinical standards.
Cleveland Clinic's health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability, and up-to-date clinical standards.
When a brain injury or another neurological condition affects your eyes, you’ll want the best care. Cleveland Clinic’s neuro-ophthalmology experts can help.
