Urge incontinence is a type of urinary incontinence that causes an urgent, uncontrollable need to pee several times during the day and night. You may leak pee before you get to the bathroom. An overactive bladder causes urge incontinence. Treatment may include Kegel exercises and therapies like botulinum toxin and nerve stimulation.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
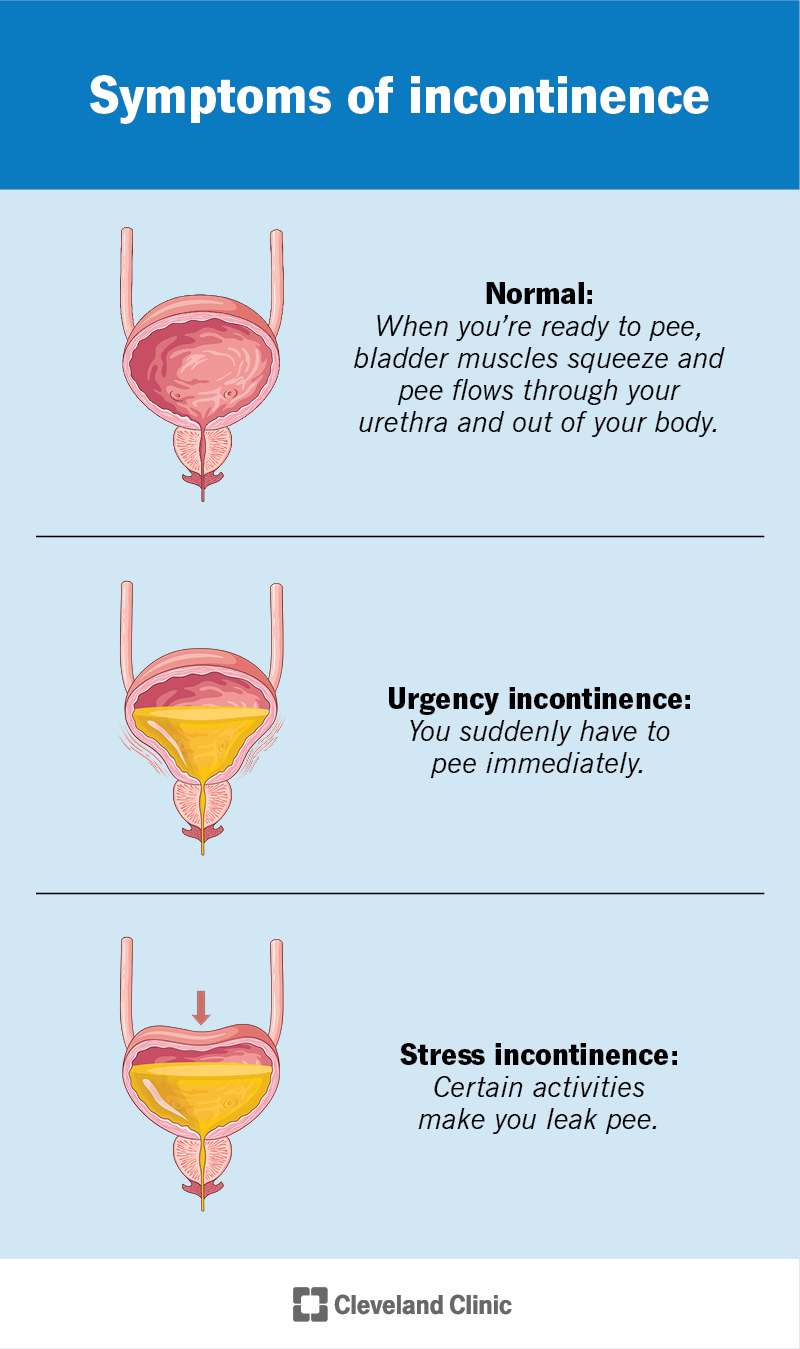
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/urge-incontinence)
Urge incontinence is a type of urinary incontinence or leakage. It causes a sudden urge to urinate (pee) and you can’t hold it. You may accidentally leak pee before you make it to the bathroom. Some people who have urinary incontinence pee more than eight times while they’re awake and get up several times while they’re asleep to pee.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
There are different types of urinary incontinence. All of them cause you to leak pee. They include:
Approximately 40% of females and 30% of males experience urge incontinence at some point in their lives.
The most common cause of urge incontinence is an overactive bladder. An overactive bladder causes muscles in your bladder to squeeze (contract) more than they should. This makes you feel like you have to pee before your bladder is actually full.
A squeezed bladder also causes the sphincter muscle inside your urethra to relax. When this muscle opens, it lets pee leak out.
Advertisement
The main sign of urge incontinence is an urgent, uncontrollable need to pee that results in leakage.
Other symptoms of overactive bladder include:
Urge incontinence can also affect your mental health. Some people with severe urge incontinence may be afraid to go out in public. They may worry about being too far from a restroom or not knowing where the nearest restroom is when they have an urge to pee. These worries may increase your risk of stress, anxiety and depression.
Females are twice as likely to have urge incontinence. And it gets more common as you get older. But healthcare providers don’t consider it a normal part of aging. That means treatment is possible.
Other risk factors for urge incontinence include:
It’s possible you’ve had mild urge incontinence symptoms for a while. Over time, overactive bladder symptoms can get worse and become more noticeable. Contact a healthcare provider if urge incontinence symptoms develop after a recent medical procedure, injury or the start of a new medication. A nerve injury or another problem may be causing urge incontinence.
A healthcare provider will review your medical history and ask about your symptoms to diagnose urge incontinence. Additional workup will include a physical exam. This may include a pelvic exam if you have a vagina or a digital rectal exam if you have a prostate. To help your provider make an accurate diagnosis, they may ask you to keep a bladder diary for two to three days. In your bladder diary, you’ll record:
Your provider may also order tests, including:
Advertisement
Urge incontinence usually doesn’t go away on its own. But treatments can help alleviate your symptoms.
Urge incontinence treatment depends on the severity of your symptoms. A healthcare provider may ask questions to determine how much urge incontinence affects your life, including:
According to your responses and the results of any testing, a provider may recommend the following:
Kegel exercises (pelvic floor exercises) help strengthen the muscles that support your urinary system, which can improve your symptoms.
It’s important to target and use the correct muscles. This can be more difficult than you might think. A physical therapist who specializes in pelvic floor disorders can teach you the proper techniques. They can also use biofeedback to ensure you get the most benefit from the exercises. It can take up to four to six weeks of regular pelvic floor exercises to see improvements in your urge incontinence symptoms.
Advertisement
It’s also possible that spasms or excess tension in your pelvic floor muscles can make overactive bladder symptoms worse. In this case, a pelvic floor physical therapist can teach you how to relax and coordinate these muscles.
Bladder retraining involves only using the restroom at set times. The goal is to wait a little longer between when you pee, even if you really have to go. This helps build up your pelvic floor muscle strength so you can hold your pee longer and longer.
Some people require timed voiding and pee more often. If you don’t get an urgency to pee until your bladder is very full, it may be too late. If you try to go more often, like every two hours, you’ll keep your bladder emptier and are less likely to have a leakage problem.
Lifestyle changes that can help ease urge incontinence include:
Advertisement
If bladder retraining and lifestyle changes don’t help, a healthcare provider may recommend:
Botox helps relax your bladder muscles so it can hold more pee. But it isn’t permanent. You’ll need additional injections as it wears off and your muscles contract again, about every six months.
There are three approaches to gently stimulating the nerves that supply your bladder. This helps regulate how your nervous system communicates with your bladder. These approaches include:
Urge incontinence can cause you a lot of stress. At-home therapies, like Kegel exercises and bladder retraining, can help reduce urge incontinence. But it may take over a month or more before you notice any changes, and your symptoms may never completely disappear. It’s important to talk to a healthcare provider. They can tell you how severe your case is and recommend the best ways to manage urge incontinence so it has the smallest possible impact on your life.
Without treatment, urge incontinence can get worse. You may have to go to the bathroom more often or leak larger amounts of pee. These problems are more likely to occur if you smoke or don’t maintain a healthy weight for you.
The same steps that help treat urge incontinence can also help prevent it. These include:
Because urge incontinence causes you to leak pee, you may want to wear absorbent underwear or urinary pads until treatments take effect. Unfortunately, constant exposure to pee can lead to skin rashes (diaper rash) and sores. To protect your skin, it’s a good idea to apply a layer of petroleum jelly (Vaseline®). If irritation doesn’t go away with just petroleum jelly, you can try a cream or ointment that contains zinc oxide and see a healthcare provider.
If urge incontinence causes you stress, depression or anxiety, it can be helpful to talk to a therapist (counselor) or psychologist. They can help you manage your mental health.
Talk to a healthcare provider when you first notice symptoms of urge incontinence or changes in your bathroom habits. They can help determine what’s causing urge incontinence and help treat it or manage your symptoms. It’s also important to make sure you don’t have an active bladder infection (UTI) if your symptoms become worse.
You may want to ask your healthcare provider:
Urge incontinence and stress incontinence have different causes and symptoms:
Talking about your bathroom habits can be embarrassing, so it’s easy to feel like you’re the only person with urge incontinence. But you’re not alone. Urge incontinence affects many people at some point in their lives. Telling trusted family members or friends can help them understand any changes in your behavior. They can also help reduce urge incontinence’s impact on your life by helping you identify public restrooms before you need to go or distracting others if you take longer than usual in the bathroom.
It’s also important to talk to a healthcare provider about the best possible treatment for your situation. With treatment, prior planning and help from others, you can help reduce the effect urge incontinence has on your life.

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
It can be stressful (and painful) to have bladder disorders, like urinary incontinence or cystitis. But the urology providers at Cleveland Clinic are here for you.
