Familial hypercholesterolemia (FH) is a genetic disorder that increases your risk of heart disease at a younger age than usual. Treatments like cholesterol-lowering medications and changes in what you eat can cut down your risk by more than half. Letting your family know you have FH gives them the chance to get tested and get early treatment.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
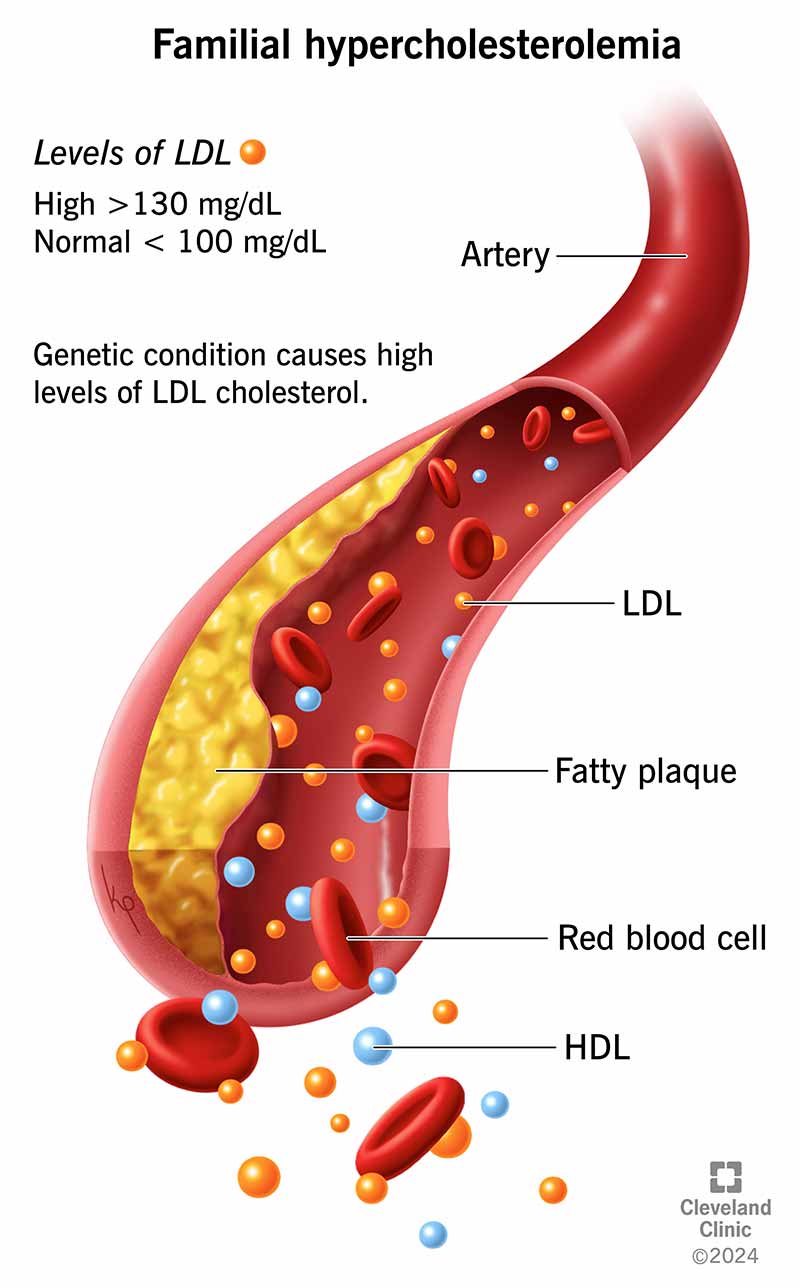
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/22067-familial-hypercholesterolemia-illustration)
Familial hypercholesterolemia (FH) is a genetic disorder that gives you very high levels of low-density lipoprotein (LDL) cholesterol. LDL is the “bad” cholesterol that can lead to cholesterol plaque buildup in your arteries. This can eventually cause heart attacks, strokes or peripheral artery disease.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
A healthy LDL level is less than 100 mg/dL (milligrams per deciliter). People with familial hypercholesterolemia can have an LDL of 160mg/dL or higher.
Without treatment, people who have this disorder are at a higher risk of getting coronary artery disease early. This can lead to heart attacks and other cardiovascular issues at a much younger age than for people who don’t have FH.
While this may sound overwhelming, there is hope. You can treat familial hypercholesterolemia by taking medicines and changing daily habits.
There are two types of FH. The difference between them is in whether one or both biological parents give you the genetic variant (change) that causes FH:
FH is an autosomal dominant genetic disorder, which means it only takes one parent to pass it on.
About 1 in 250 people have a genetic variant for the more common type of familial hypercholesterolemia. Only 1 in 250,000 people have the more severe type.
Advertisement
Most people — 9 out of 10 — who have FH don’t know they have it.
You may not notice symptoms of familial hypercholesterolemia until you have coronary artery disease. But people with FH need treatment much earlier than that because their LDL level starts out high even as newborns.
This condition leads to LDL cholesterol buildup, which can cause familial hypercholesterolemia symptoms like:
FH is a genetic disorder you inherit or get from one or both of your biological parents. In most people with this genetic issue, a specific protein (LDL receptor) that gets LDL out of your blood doesn’t work well or there isn’t enough of it.
Although most people with familial hypercholesterolemia will have a variant on one of three specific genes (APOB, LDLR or PCSK9), researchers are still discovering more. If you appear to have familial hypercholesterolemia but test negative for it, you may have gotten it from a genetic variant that researchers haven’t identified yet.
It’s common for people who have FH to have atherosclerosis, or plaque (atheroma) collecting in their arteries. This can lead to:
Early treatment greatly reduces your risk of these complications.
Your healthcare provider can make a familial hypercholesterolemia diagnosis based on:
A provider can use a lipid panel or DNA test to make a familial hypercholesterolemia diagnosis.
A lipid panel blood test measures your cholesterol levels, including your LDL cholesterol. Children with familial hypercholesterolemia can have LDL levels higher than 160 mg/dL. Adults can have LDL of 190 mg/dL or higher. In people with the severe form, homozygous familial hypercholesterolemia, LDL can be higher than 400 mg/dL.
Advertisement
A DNA test can find problems with one of the three genes researchers know can cause FH.
After you get an FH diagnosis, you can expect to see your provider regularly to check on your cardiovascular health.
Familial hypercholesterolemia treatment may include one or more medications to reduce your LDL level as low as possible. People with severe FH may need periodic LDL apheresis (blood filtering) or a liver transplant (rarely).
Medicines for this type include:
Medications for this type include:
People with familial hypercholesterolemia have a much higher risk of atherosclerosis, which can cause heart attacks and strokes. Without treatment, people who have FH have 20 times the risk of coronary artery disease compared to someone without the disease. The chances of getting coronary artery disease go up even more if you use tobacco products, have diabetes or other risk factors for cardiovascular disease.
Without early treatment, heart disease can start before age 10 for people who have homozygous FH. People with the heterozygous type may develop heart disease at age 30 without treatment. For either type, this can lead to a heart attack by age 50 or 60 (depending on your sex).
Advertisement
Since FH is a condition you inherit from your parents, it’s a part of your DNA all your life. You’ll need lifelong treatment.
Healthcare providers don’t have a cure for familial hypercholesterolemia. But once you know you have FH, your provider can treat you for it and help you prevent cardiovascular disease. With early treatment for FH, the outlook (prognosis) is excellent.
You can most likely have a normal life expectancy if you know your risk at a younger age and get treatment. Getting treatment for familial hypercholesterolemia cuts down your risk of heart disease by more than half. Without treatment, people with the rare type of FH may not live to be 30.
You can’t prevent an inherited disease like familial hypercholesterolemia. But you can help your family get treatment early by letting them know about your diagnosis.
People with FH are at a higher risk of heart disease at a younger age than those without FH. If you have familial hypercholesterolemia, your biological siblings, parents and children should get a test. You can start screening a child at age 2 if they have a high risk of FH.
If you have familial hypercholesterolemia, you can lower your risk of cardiovascular problems in these ways:
Advertisement
If you have familial hypercholesterolemia, your top goal is to cut down your LDL level. Ways to achieve this — before or in addition to taking medicine — include eating:
Regular appointments with your healthcare provider are crucial to make sure your medication is working. Contact your provider if you’re having trouble with side effects from your medicine. They may be able to switch you to a different one.
Get help immediately if you have chest pain, shortness of breath or another symptom of a heart attack or stroke.
Questions to ask your provider include:
You may feel scared or discouraged when you find out you have familial hypercholesterolemia. But getting a diagnosis is the first step toward lowering your risk of heart attack and stroke. Going to regular appointments with your healthcare provider will help them keep tabs on how you’re doing with the medicines they prescribe for you. Eating foods low in saturated and trans fats can help, as well as being physically active and addressing other risk factors for heart disease.

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s primary care providers offer lifelong medical care. From sinus infections and high blood pressure to preventive screening, we’re here for you.
