Raynaud’s syndrome causes spasms in small blood vessels in your fingers and toes. This limits blood flow and leads to symptoms like skin color changes, cold skin and a pins and needles sensation. Common triggers of Raynaud’s attacks include cold weather and stress. Many people have mild symptoms that they can manage through lifestyle changes.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Raynaud’s (pronounced ray-nodes) syndrome is a disorder that affects small blood vessels in your fingers and toes. It may also affect blood vessels in your nose, lips or ear lobes. Raynaud’s causes you to have episodic spasms, called vasospastic attacks, in response to cold temperatures or stress.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
During a Raynaud’s attack, the arterioles and capillaries in your fingers and toes tighten more than they should. As a result, your skin in the affected area turns white and then blue. This color change happens because your blood lacks oxygen. Your skin may also feel cold or numb. As your blood vessels relax and open up again, your skin may look red or feel tingly. An attack usually lasts around 15 minutes.
There are two main types of Raynaud’s syndrome:
The chart below lists what you should know about each type.
| Feature | Raynaud’s disease (primary) | Raynaud’s phenomenon (secondary) |
|---|---|---|
| Cause | Unknown. Not linked with an underlying disease. | Underlying disease, condition, medication or lifestyle factor. |
| Symptoms | Usually mild (skin color changes, numbness, pins and needles). Doesn’t cause skin ulcers or gangrene. | May be mild or more severe. May cause skin ulcers or gangrene. |
| Prevalence | More common. | Less common. |
| Treatment | Lifestyle changes. | Targets underlying cause. May include medications or procedures. |
| Feature | ||
| Cause | ||
| Raynaud’s disease (primary) | ||
| Unknown. Not linked with an underlying disease. | ||
| Raynaud’s phenomenon (secondary) | ||
| Underlying disease, condition, medication or lifestyle factor. | ||
| Symptoms | ||
| Raynaud’s disease (primary) | ||
| Usually mild (skin color changes, numbness, pins and needles). Doesn’t cause skin ulcers or gangrene. | ||
| Raynaud’s phenomenon (secondary) | ||
| May be mild or more severe. May cause skin ulcers or gangrene. | ||
| Prevalence | ||
| Raynaud’s disease (primary) | ||
| More common. | ||
| Raynaud’s phenomenon (secondary) | ||
| Less common. | ||
| Treatment | ||
| Raynaud’s disease (primary) | ||
| Lifestyle changes. | ||
| Raynaud’s phenomenon (secondary) | ||
| Targets underlying cause. May include medications or procedures. |
Most people use these terms interchangeably. But scientists use them to distinguish between primary and secondary forms of the condition.
Primary Raynaud’s syndrome isn’t serious and doesn’t damage your blood vessels. It may disrupt some of your daily activities, but it’s not dangerous.
Advertisement
Secondary Raynaud’s syndrome can be more serious. It may lead to skin ulcers and, rarely, tissue death (gangrene). It may also impact your quality of life. The underlying disease causing it may be severe in and of itself.
Primary Raynaud’s syndrome usually affects:
Secondary Raynaud’s syndrome usually affects people who have another disease or condition. It can also affect people who perform a job that puts repetitive pressure on their hands. Here are some facts to know:
Raynaud’s syndrome is common. Estimates vary, but Raynaud’s likely affects up to 1 in 20 people in the U.S.
Raynaud’s syndrome is an exaggerated version of a normal body process called vasomotor response. Vasomotor response means your blood vessels open up (vasodilation) and tighten (vasoconstriction) to help your body respond to its environment.
For example, if it’s cold outside, blood vessels near your skin’s surface constrict to move blood to veins deeper in your body. This allows your body to conserve heat. Your blood vessels also constrict when you’re stressed to help your body save oxygen.
Raynaud’s disrupts this normal body process and causes your blood vessels to constrict more than they should. This interrupts your normal blood flow and limits the oxygen available to your fingers or toes.
Primary Raynaud’s syndrome doesn’t affect your heart. But conditions associated with secondary Raynaud’s syndrome may affect your heart. Talk with your healthcare provider to learn if your condition affects your heart.
Raynaud’s symptoms affect your skin and may include:
Advertisement
Symptoms of Raynaud’s syndrome are episodic. That means they come and go. A typical episode, or attack, lasts about 15 minutes. But attacks may be shorter or longer. Episodes are often associated with certain triggers such as cold weather. Symptoms are usually mild in people with primary Raynaud’s syndrome. People with secondary Raynaud’s syndrome may have more severe symptoms, including skin ulcers.
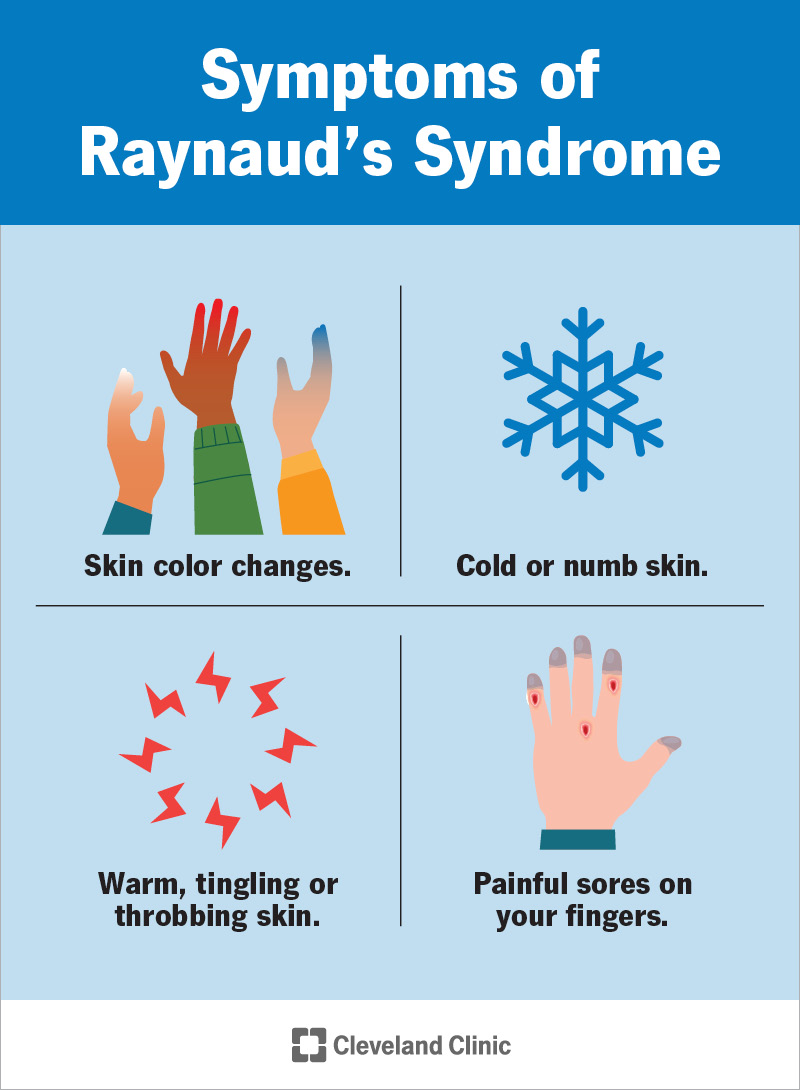
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/9849-raynauds-syndrome.jpg)
Raynaud’s can cause your skin to change color briefly . It may first look white before turning blue then red. Your skin may also feel cold or numb at the start of an attack due to reduced blood flow. When blood flow returns, your fingers may feel warm or throb.
Triggers that can lead to a Raynaud’s attack include:
Primary Raynaud’s syndrome has no identifiable underlying cause.
An underlying disease or condition usually causes secondary Raynaud’s syndrome (Raynaud’s phenomenon). It’s especially common in people with connective tissue diseases. Some of these diseases reduce blood flow to your fingers and toes.
Advertisement
Other causes include repetitive motions and some medications. The lists below break down the many causes of Raynaud’s phenomenon.
Healthcare providers can typically diagnose Raynaud’s syndrome from your symptoms. Your provider may ask you to take photos of your skin changes when they happen. Your provider may also perform a physical exam and talk with you about your medical and family history.
Advertisement
Raynaud’s syndrome is usually easy to diagnose. But it may not be obvious whether you have the primary or secondary form. That’s where diagnostic testing can help.
Several diagnostic tests can help determine if you have primary or secondary Raynaud’s syndrome.
One test that’s particularly useful is a nailfold capillaroscopy. For this test, your provider places a drop of oil on your skin at the base of your fingernail. This spot is called your nailfold. Your provider then looks at your nailfold under a microscope. If your capillaries in the area are enlarged or abnormal, you may have a connective tissue disease. This would indicate you likely have secondary Raynaud’s syndrome.
Other tests your provider may order include:
These tests can help your provider identify or rule out underlying conditions as causes of your Raynaud’s symptoms.
You may receive care from healthcare providers in different specialties. That’s because Raynaud’s syndrome can affect your body in many ways. It can also result from a wide range of medical conditions. Providers who may help with your diagnosis and treatment include:
Treatment depends on the severity of your condition and whether you have the primary or secondary form. Treatment goals include:
For many people, lifestyle changes are enough to manage their condition. These include:
However, if you have severe symptoms, you may need medication. Your provider may prescribe one or more of the following medications:
If you have severe Raynaud’s and other treatment methods don’t work, your provider may recommend a procedure called a sympathectomy. A sympathectomy temporarily blocks or cuts tiny nerves near your affected blood vessels. This prevents the nerves from sending signals that make your blood vessels get too narrow. The procedure should relieve your symptoms for one or two years, but you may need it again in the future.
For most people with primary Raynaud’s syndrome, the outlook is positive. Symptoms may bother you off and on, but the condition isn’t serious or life-threatening. Over time, you’ll learn more self-care tips for preventing attacks or helping them go away.
If you have secondary Raynaud’s syndrome, your outlook depends on your underlying disease. Talk with your provider about what you can expect and how to manage your condition.
There’s nothing you can do to prevent Raynaud’s syndrome. But you can help prevent attacks by learning your triggers and taking action to avoid them.
It’s also important to visit your provider for yearly checkups. Doing so can help your provider diagnose and treat underlying conditions that may cause Raynaud’s phenomenon. Some of these conditions are preventable with lifestyle changes, such as avoiding tobacco products.
Self-care is essential for managing Raynaud’s syndrome. Follow your healthcare provider’s guidance on how to avoid triggers and how to manage an attack when it happens. The following tips can also help.
Also, it’s important to know which medications can trigger an attack. Ask your provider if any of your current medications could cause your condition to flare up. These include some medications that treat:
If an attack does happen, be proactive. Don’t ignore a Raynaud’s attack or assume it’ll go away on its own. Taking the proper steps can reduce the length and severity of an attack. Here’s what to do:
Call your provider if you:
As with any condition, see your provider any time you’re worried, frightened or have questions about how to care for yourself.
Primary Raynaud’s disease often begins during the teenage years. Rarely, it can begin earlier. So, if your child or teen starts to have symptoms, take them to see their healthcare provider. Their provider may want to run tests to rule out an underlying condition.
Usually, Raynaud’s in kids and teens is mild, and symptoms should ease as your child gets older. The same management tips for adults also can help your child. For example, dress your child warmly in cold weather (and give them two pairs of mittens to wear rather than just one). Keep your home and car warm, and avoid air conditioning that’s too cold.
It’s also important to tell administrators at your child’s school about their condition. Your child may need special permission to avoid outdoor activities (like gym class) during the colder months.
Raynaud’s syndrome is a common condition that may affect your quality of life. Learning how to care for yourself at home can help you avoid and manage Raynaud’s attacks. If your symptoms are preventing you from doing the things you love, talk with your provider about treatment options. It may also help to connect with a support group to learn from others living with the same condition.

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s primary care providers offer lifelong medical care. From sinus infections and high blood pressure to preventive screening, we’re here for you.
