A cavernous malformation, also known as cavernoma or cavernous hemangioma, is an abnormal tangle of blood vessels. These are usually found in your brain, brainstem and spinal cord. The thin walls of these malformations may bleed, which can cause seizures or a stroke. Treatments include observation, medications and surgery.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
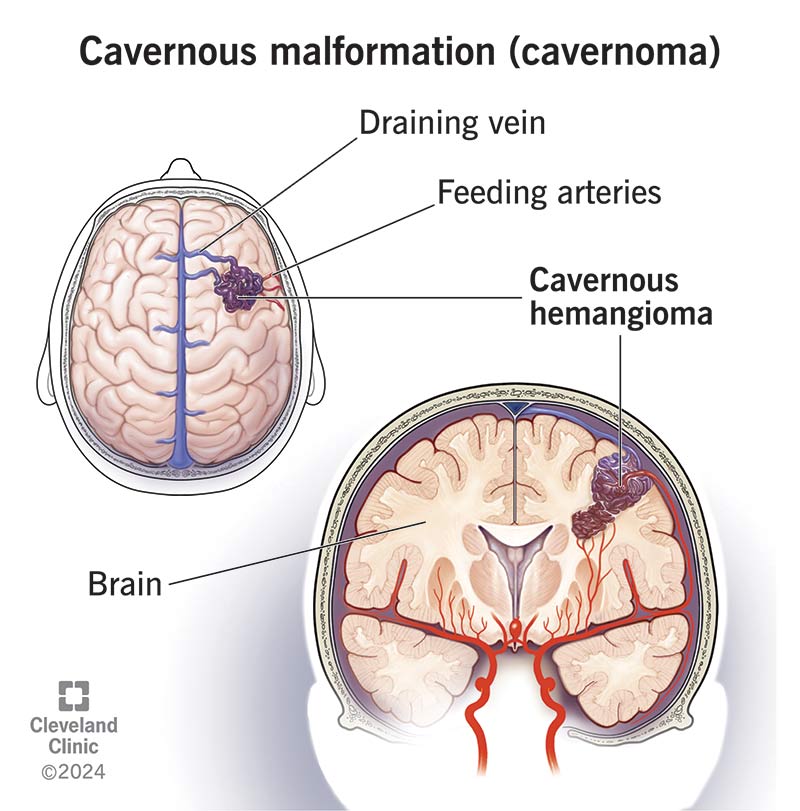
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/cavernous-hemangioma)
A cavernous malformation is an abnormal cluster of tightly packed capillaries (small blood vessels). It’s usually located in your brain, brainstem and spinal cord (cerebral cavernous malformation).
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
The cavernous hemangioma (lesion) looks like a raspberry. It can range in size from a fraction of an inch to dime-sized or larger. It has blood-filled spaces with connective tissues between them. They don’t have a lot of support and they’re thinner than other capillaries. This makes them more likely to leak blood. As a result, you may experience symptoms and potentially life-threatening complications if the bleed is severe.
Cavernous malformations go by many different names. You may hear your healthcare provider refer to them as:
The thin walls of these capillaries make cerebral cavernous malformations prone to bleeding. Bleeding in your brain and spinal cord (hemorrhage) can cause seizures, paralysis or stroke. They can be life-threatening in severe cases. But most hemangiomas don’t cause too many problems.
Many factors determine if cavernous malformations are dangerous, including:
Because each person’s situation is unique, it’s best to ask your healthcare provider about your risk for dangerous and possibly life-threatening events.
Advertisement
Symptoms may include:
Symptoms usually appear between ages 20 and 60. You might not experience any symptoms. If you do have symptoms, it’s usually a sign that the cavernoma is bleeding. But you also might not have any symptoms during a bleed. They range in severity based on the size and location.
Cavernous malformations can develop anywhere in your body. They usually only cause serious problems in your brain or spinal cord. They can also appear on your skin, liver and eyes.
Healthcare providers aren’t sure what causes most cavernous malformations. Nearly 20% are genetic and happen due to a variant of the following genes:
These genes produce proteins that connect blood vessel cells to each other (junctions). A genetic variant weakens the cell junction and causes hemangiomas to form.
Some cavernous malformations are hereditary (run in families). Having more than one cerebral cavernous hemangioma is more common in people with a family history.
You could receive one copy of the gene variant from a biological parent to inherit this condition (autosomal dominant). If you have a hemangioma, your children have about a 50% chance of having one, too.
But most cases happen sporadically (randomly), without any genetic history of the condition in your biological family.
You may be more at risk of a cerebral cavernous malformation if you:
A healthcare provider will diagnose a cerebral cavernous malformation after an exam and testing. Your provider will review your symptoms during a physical exam. They may offer a genetic test to find a genetic variant that caused the cavernoma. Your provider may also offer an MRI to see the malformation more closely and look for signs of bleeding or swelling.
Your provider may order a special type of MRI scan called susceptibility-weighted imaging. This is a more sensitive type of MRI. It detects the tiniest cavernous hemangiomas, as well as remnants of prior bleeds. This information helps give your care team some idea about the risk of future complications.
Advertisement
Providers typically don’t diagnose cerebral cavernous malformations until they rupture and bleed. However, you may have a cavernoma without symptoms. In this case, your provider would diagnose it if you had a brain scan for another reason.
Cavernous malformation treatment varies based on its location and whether or not it’s bleeding or causing symptoms.
If the cavernoma isn’t bleeding, your provider may schedule regular imaging scans to monitor it over time. You’ll also learn more about what symptoms to look out for and when to call your provider in case a bleed occurs between appointments.
Your provider may recommend the following treatment options for a bleeding cavernous malformation:
Your provider may consider surgery if:
Cerebral cavernous malformation bleeds and ruptures aren’t common, but they do happen. Research estimates that you have a 2.4% chance of having a bleed annually if you have one.
Advertisement
Treatment options are available. While there are risks to surgery, the outcome of removing a cerebral cavernous malformation is usually successful if your surgeon can safely access it.
If you have more than one hemangioma or one that’s bleeding or causing symptoms, your provider will discuss how often to have follow-up MRI scans.
Yes, if you had a bleed, you’re at a higher risk of a future bleed. A healthcare provider will let you know how to take care of yourself to help prevent future bleeds.
Cerebral cavernous malformations can be life-threatening if they cause severe bleeding. But most don’t affect life expectancy. Complications after a bleed, however, may affect your quality of life, like after a stroke.
Each person’s situation is different. You should speak with your healthcare provider to learn more about your situation.
There’s no known way to prevent cavernous malformations. If you have a family history of these hemangiomas, your provider will discuss genetic testing and genetic counseling to help you learn more about this condition.
While you can’t prevent all cavernoma bleeds or ruptures, you can reduce your risk by taking care of your general health. You can do this by:
Advertisement
Contact emergency services if you notice symptoms of a cavernous malformation, especially a first-time seizure, one-sided weakness or sudden vision changes. Symptoms may be a sign of bleeding, which could cause a stroke, so it’s important that you get care right away.
Another common type of blood vessel malformation is an arteriovenous malformation (AVM). Unlike cavernous malformations, which are filled with slow-moving or stagnant (not moving) blood, AVMs involve high-pressure blood flow.
Cavernous malformations and AVMs can be similar in size, depending on the number of blood vessels involved. They can both rupture and bleed. But if they do bleed, the high-pressure blood flow of an AVM can be more severe and cause more damage.
After AVMs, cavernous malformations are the most likely type of blood vessel lesion to need treatment. Surgery, as well as other options, is available for treating AVMs. Cavernous malformations are best treated with surgery to remove the hemangioma.
Hearing that you have a cerebral cavernous malformation can be difficult and scary. Your experience with a hemangioma is different from what happens to someone else. Your provider may recommend getting an annual MRI, managing your symptoms with medications or undergoing surgery to prevent complications.
No matter what your situation looks like, know that you’ll be surrounded by a supportive care team who’ll be with you every step of the way. They can answer any questions you might have about your diagnosis and treatment plan so you can manage this condition.

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
If you have a neurological condition, you want expert advice. At Cleveland Clinic, we’ll work to create a treatment plan that’s right for you.
